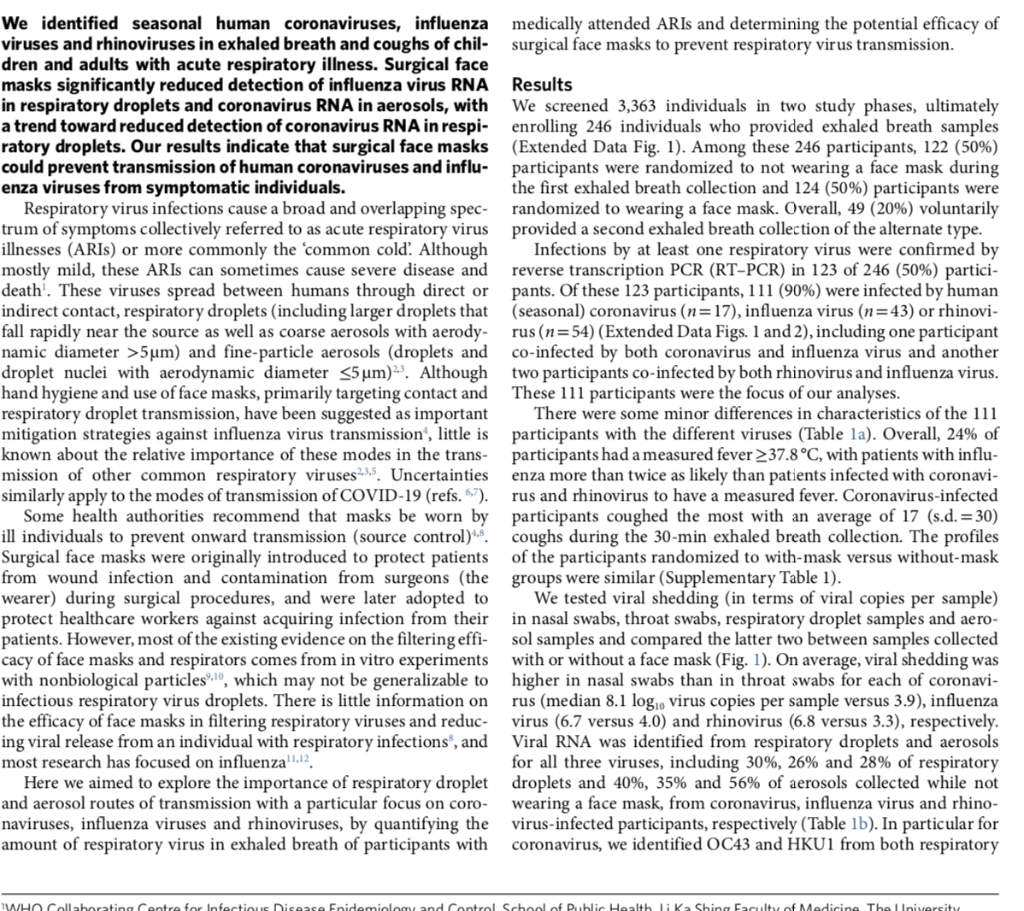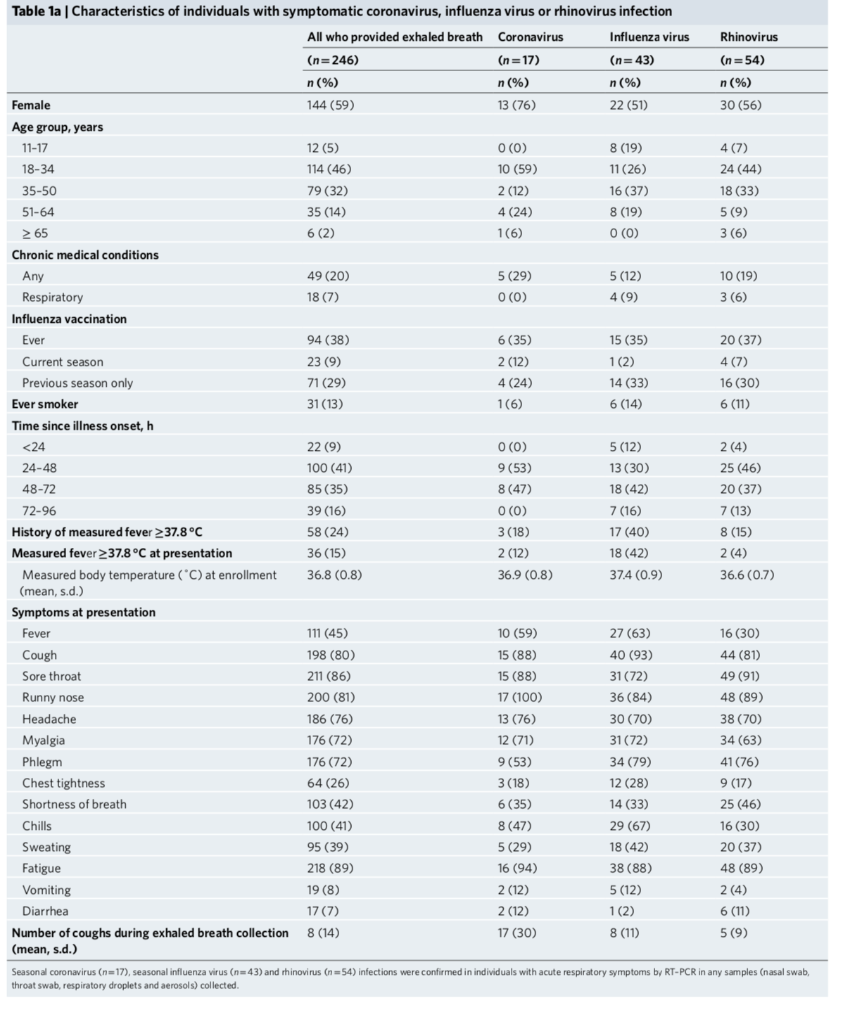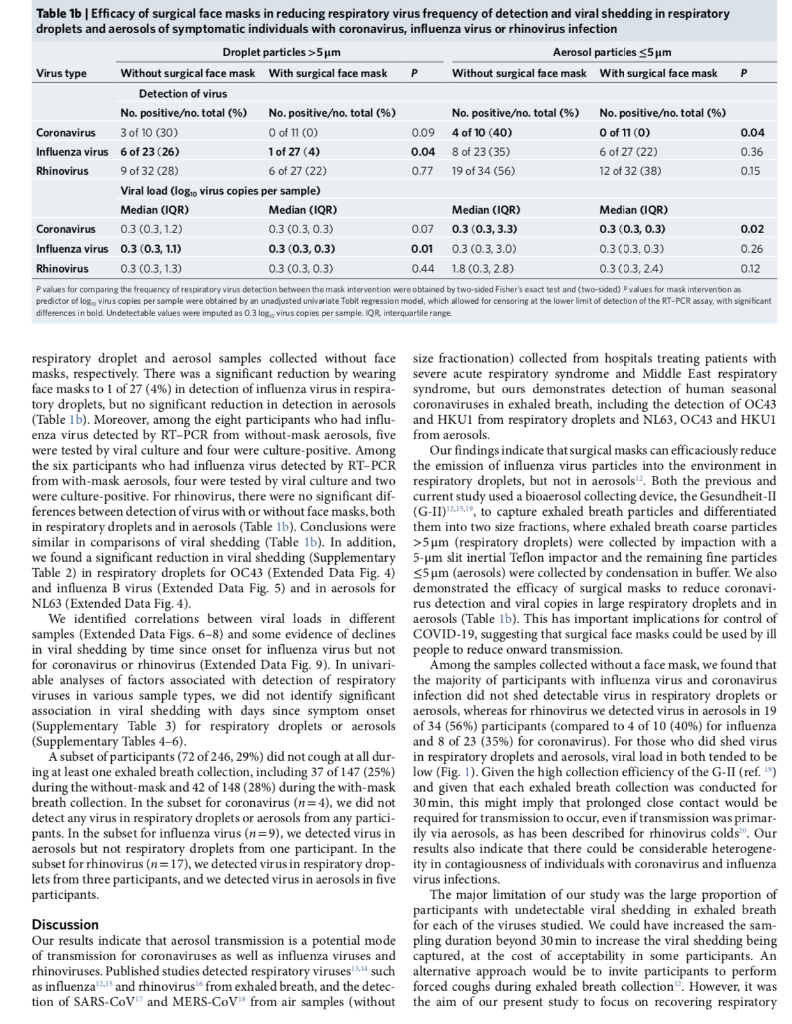
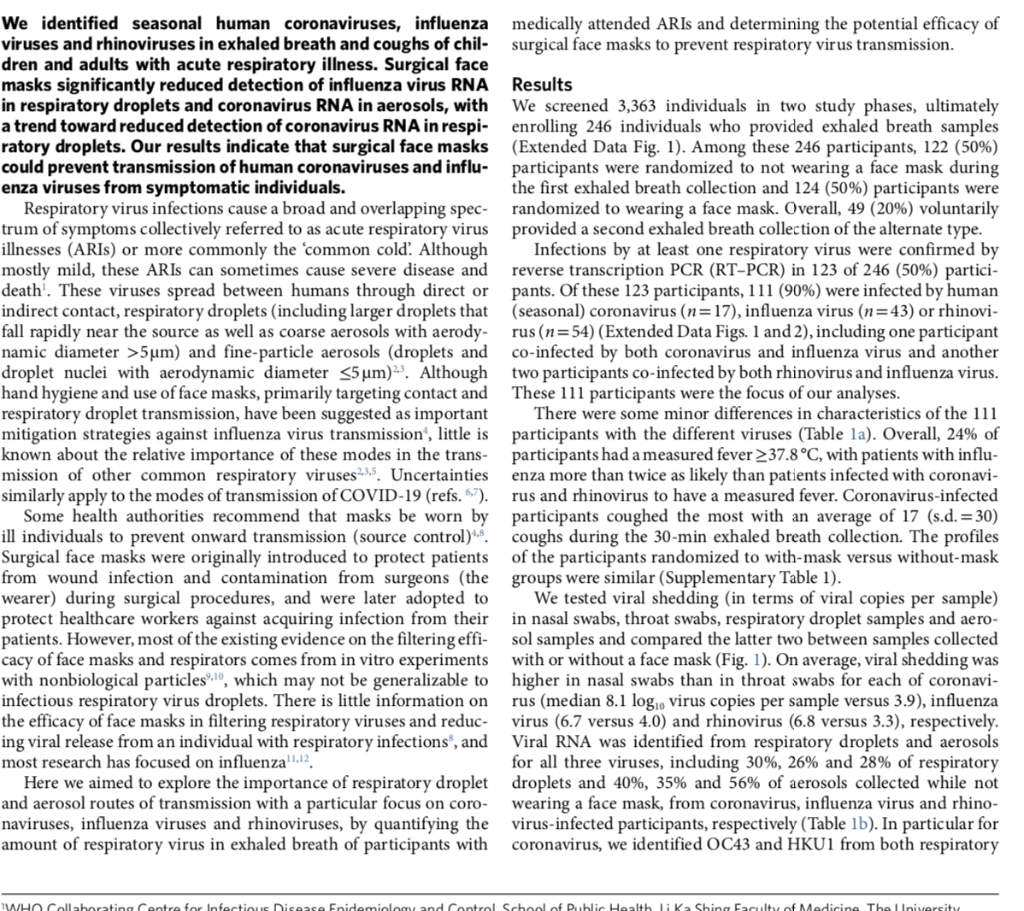
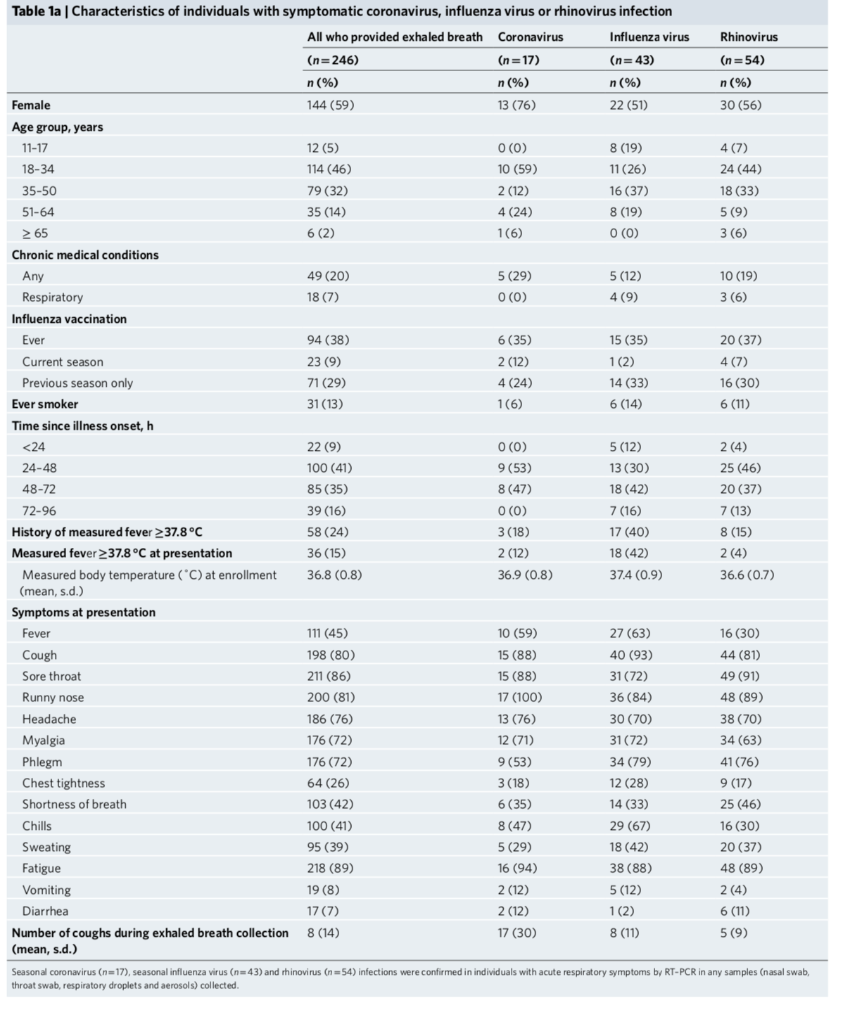
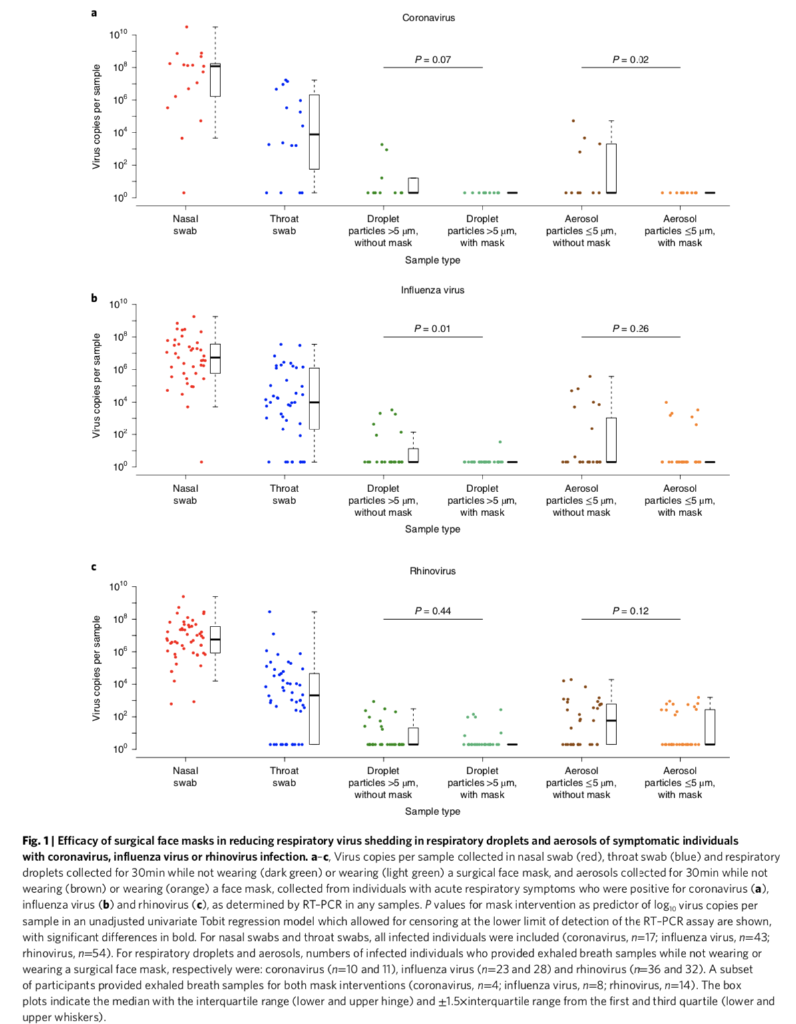
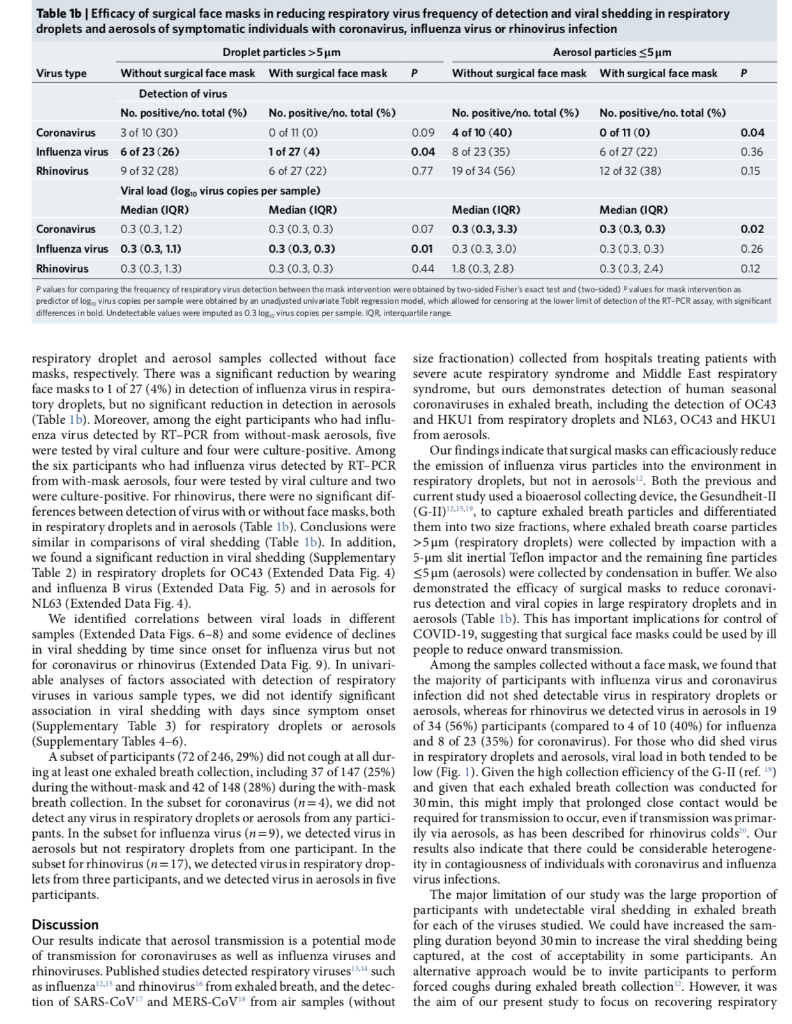
1) As a first step in data analysis, you want to make sure no outliers are present in your data set. Please describe the method that you have been taught to detect outliers by using quartiles. If we knew our date set is approximately normally distributed could you please offer an alternative way that uses mean and standard deviation of your data set? (3 Marks) 2) A consumer organization wants to know if using a certain fuel additive increases fuel efficiency in miles per gallon, or mpg). A total of 20 cars of different types and models are available for testing. Design an experiment to investigate this question. Imagine that you have access to a car test track for your experiment. Note: There is no single correct answer to this question; different students might consider different designs. Please indicate the advantage and disadvantage of your method. You should also mention the variable that you are going to measure, state your hypothesis, how you are going to run the experiment and type of statistical test you will run on your data. (3 Marks) Please read the following paper and answer the subsequent questions: Respiratory virus shedding in exhaled breath and efficacy of face masks Leung NHL et al. Nature Medicine, 2020. Note: You don't need to understand the entire paper to be able to answer these questions. Virus shedding in this case means, the number of virus measured in a sample. 3) On average, viral shedding was higher in nasal swabs than in throat swabs for each of coronavirus (median 8.1 log10 virus copies per sample versus 3.9). Middle of fourth paragraph of results and red dots in left panel of Fig. 1.a. Explain what the median of nasal swab represents? If the authors reported mean instead of median do you expect it to be higher or lower than reported median and why? How about the mode of that data set? (2 Marks) 4) Could you please explain what is shown on Fig. 1.a (left, middle and right panels)? (1.5 Marks) 5) In Fig.1, most of box and whisker plots either don't have one of their whiskers or both whiskers are missing (for example Fig. 1a right and middle panel). Could you please explain why this is the case? (0.5 Mark) 6) Refer to Fig. 1.a, could you please state null and alternative hypothesis that was tested both for droplets and for aerosol? (2 Marks) We identified seasonal human coronaviruses, influenza medically attended ARIs and determining the potential efficacy of viruses and rhinoviruses in exhaled breath and coughs of chil- surgical face masks to prevent respiratory virus transmission. dren and adults with acute respiratory illness. Surgical face masks significantly reduced detection of influenza virus RNA Results in respiratory droplets and coronavirus RNA in aerosols, with We screened 3,363 individuals in two study phases, ultimately a trend toward reduced detection of coronavirus RNA in respi- enrolling 246 individuals who provided exhaled breath samples ratory droplets. Our results indicate that surgical face masks (Extended Data Fig. 1). Among these 246 participants, 122 (50%) could prevent transmission of human coronaviruses and influ- participants were randomized to not wearing a face mask during enza viruses from symptomatic individuals. the first exhaled breath collection and 124 (50%) participants were Respiratory virus infections cause a broad and overlapping spec- randomized to wearing a face mask. Overall, 49 (20%) voluntarily trum of symptoms collectively referred to as acute respiratory virus provided a second exhaled breath collection of the alternate type. illnesses (ARIS) or more commonly the 'common cold. Although Infections by at least one respiratory virus were confirmed by mostly mild, these ARIs can sometimes cause severe disease and reverse transcription PCR (RT-PCR) in 123 of 246 (50%) partici- death. These viruses spread between humans through direct or pants. Of these 123 participants, 111 (90%) were infected by human indirect contact, respiratory droplets (including larger droplets that (seasonal) coronavirus (n=17), influenza virus (n=43) or rhinovi- fall rapidly near the source as well as coarse aerosols with aerody- rus (n=54) (Extended Data Figs. 1 and 2), including one participant namic diameter >5um) and fine particle aerosols (droplets and co-infected by both coronavirus and influenza virus and another droplet nuclei with aerodynamic diameter 5 um, particles >5 um, without mask with mask Sample type Aerosol particles s5 um, without mask Aerosol particles sum, with mask Influenza virus P. 0.01 P=0.26 Virus copies per sample Nasal swab Throat swab Droplet Droplet particles >5 um, particles >5 um, without mask with mask Sample type Aerosol particles s5 um, without mask Aerosol particles s5 um, with mask Rhinovirus P=0.44 P=0.12 Virus copies per sample Nasal swab Throat swab Droplet Droplet particles >5 um, particles >5 um, without mask with mask Sample type Aerosol particles s5um, without mask Aerosol particles s5 um, with mask Fig. 1 Efficacy of surgical face masks in reducing respiratory virus shedding in respiratory droplets and aerosols of symptomatic individuals with coronavirus, influenza virus or rhinovirus infection. a-c Virus copies per sample collected in nasal swab (red), throat swab (blue) and respiratory droplets collected for 30min while not wearing (dark green) or wearing (light green) a surgical face mask, and aerosols collected for 30min while not wearing (brown) or wearing (orange) a face mask, collected from individuals with acute respiratory symptoms who were positive for coronavirus (a), influenza virus (b) and rhinovirus (C), as determined by RT-PCR in any samples. P values for mask intervention as predictor of logo virus copies per sample in an unadjusted univariate Tobit regression model which allowed for censoring at the lower limit of detection of the RT-PCR assay are shown, with significant differences in bold. For nasal swabs and throat swabs, all infected individuals were included (coronavirus, n=17, influenza virus, n=43; rhinovirus, n=54). For respiratory droplets and aerosols, numbers of infected individuals who provided exhaled breath samples while not wearing or wearing a surgical face mask, respectively were: coronavirus (n=10 and 11), influenza virus (n=23 and 28) and rhinovirus (n=36 and 32). A subset of participants provided exhaled breath samples for both mask interventions (coronavirus, n=4; influenza virus, n=8; rhinovirus, n=14). The box plots indicate the median with the interquartile range (lower and upper hinge) and +1.5xinterquartile range from the first and third quartile (lower and upper whiskers). Table 1b Efficacy of surgical face masks in reducing respiratory virus frequency of detection and viral shedding in respiratory droplets and aerosols of symptomatic individuals with coronavirus, influenza virus or rhinovirus infection Droplet particles >5um Aerosol particles 5um (respiratory droplets) were collected by impaction with a 5-um slit inertial Teflon impactor and the remaining fine particles S5um (aerosols) were collected by condensation in buffer. We also demonstrated the efficacy of surgical masks to reduce coronavi- rus detection and viral copies in large respiratory droplets and in aerosols (Table 1b). This has important implications for control of COVID-19, suggesting that surgical face masks could be used by ill people to reduce onward transmission. Among the samples collected without a face mask, we found that the majority of participants with influenza virus and coronavirus infection did not shed detectable virus in respiratory droplets or aerosols, whereas for rhinovirus we detected virus in aerosols in 19 of 34 (56%) participants (compared to 4 of 10 (40%) for influenza and 8 of 23 (35%) for coronavirus). For those who did shed virus in respiratory droplets and aerosols, viral load in both tended to be low (Fig. 1). Given the high collection efficiency of the G-ll (ref." and given that each exhaled breath collection was conducted for 30 min, this might imply that prolonged close contact would be required for transmission to occur, even if transmission was primar- ily via aerosols, as has been described for rhinovirus colds. Our results also indicate that there could be considerable heterogene- ity in contagiousness of individuals with coronavirus and influenza virus infections. The major limitation of our study was the large proportion of participants with undetectable viral shedding in exhaled breath for each of the viruses studied. We could have increased the sam- pling duration beyond 30 min to increase the viral shedding being captured, at the cost of acceptability in some participants. An alternative approach would be to invite participants to perform forced coughs during exhaled breath collection. However, it was the aim of our present study to focus on recovering respiratory Discussion Our results indicate that aerosol transmission is a potential mode of transmission for coronaviruses as well as influenza viruses and rhinoviruses. Published studies detected respiratory viruses such as influenza 2.15 and rhinovirus from exhaled breath, and the detec- tion of SARS-CoV and MERS-CoV from air samples without 1) As a first step in data analysis, you want to make sure no outliers are present in your data set. Please describe the method that you have been taught to detect outliers by using quartiles. If we knew our date set is approximately normally distributed could you please offer an alternative way that uses mean and standard deviation of your data set? (3 Marks) 2) A consumer organization wants to know if using a certain fuel additive increases fuel efficiency in miles per gallon, or mpg). A total of 20 cars of different types and models are available for testing. Design an experiment to investigate this question. Imagine that you have access to a car test track for your experiment. Note: There is no single correct answer to this question; different students might consider different designs. Please indicate the advantage and disadvantage of your method. You should also mention the variable that you are going to measure, state your hypothesis, how you are going to run the experiment and type of statistical test you will run on your data. (3 Marks) Please read the following paper and answer the subsequent questions: Respiratory virus shedding in exhaled breath and efficacy of face masks Leung NHL et al. Nature Medicine, 2020. Note: You don't need to understand the entire paper to be able to answer these questions. Virus shedding in this case means, the number of virus measured in a sample. 3) On average, viral shedding was higher in nasal swabs than in throat swabs for each of coronavirus (median 8.1 log10 virus copies per sample versus 3.9). Middle of fourth paragraph of results and red dots in left panel of Fig. 1.a. Explain what the median of nasal swab represents? If the authors reported mean instead of median do you expect it to be higher or lower than reported median and why? How about the mode of that data set? (2 Marks) 4) Could you please explain what is shown on Fig. 1.a (left, middle and right panels)? (1.5 Marks) 5) In Fig.1, most of box and whisker plots either don't have one of their whiskers or both whiskers are missing (for example Fig. 1a right and middle panel). Could you please explain why this is the case? (0.5 Mark) 6) Refer to Fig. 1.a, could you please state null and alternative hypothesis that was tested both for droplets and for aerosol? (2 Marks) We identified seasonal human coronaviruses, influenza medically attended ARIs and determining the potential efficacy of viruses and rhinoviruses in exhaled breath and coughs of chil- surgical face masks to prevent respiratory virus transmission. dren and adults with acute respiratory illness. Surgical face masks significantly reduced detection of influenza virus RNA Results in respiratory droplets and coronavirus RNA in aerosols, with We screened 3,363 individuals in two study phases, ultimately a trend toward reduced detection of coronavirus RNA in respi- enrolling 246 individuals who provided exhaled breath samples ratory droplets. Our results indicate that surgical face masks (Extended Data Fig. 1). Among these 246 participants, 122 (50%) could prevent transmission of human coronaviruses and influ- participants were randomized to not wearing a face mask during enza viruses from symptomatic individuals. the first exhaled breath collection and 124 (50%) participants were Respiratory virus infections cause a broad and overlapping spec- randomized to wearing a face mask. Overall, 49 (20%) voluntarily trum of symptoms collectively referred to as acute respiratory virus provided a second exhaled breath collection of the alternate type. illnesses (ARIS) or more commonly the 'common cold. Although Infections by at least one respiratory virus were confirmed by mostly mild, these ARIs can sometimes cause severe disease and reverse transcription PCR (RT-PCR) in 123 of 246 (50%) partici- death. These viruses spread between humans through direct or pants. Of these 123 participants, 111 (90%) were infected by human indirect contact, respiratory droplets (including larger droplets that (seasonal) coronavirus (n=17), influenza virus (n=43) or rhinovi- fall rapidly near the source as well as coarse aerosols with aerody- rus (n=54) (Extended Data Figs. 1 and 2), including one participant namic diameter >5um) and fine particle aerosols (droplets and co-infected by both coronavirus and influenza virus and another droplet nuclei with aerodynamic diameter 5 um, particles >5 um, without mask with mask Sample type Aerosol particles s5 um, without mask Aerosol particles sum, with mask Influenza virus P. 0.01 P=0.26 Virus copies per sample Nasal swab Throat swab Droplet Droplet particles >5 um, particles >5 um, without mask with mask Sample type Aerosol particles s5 um, without mask Aerosol particles s5 um, with mask Rhinovirus P=0.44 P=0.12 Virus copies per sample Nasal swab Throat swab Droplet Droplet particles >5 um, particles >5 um, without mask with mask Sample type Aerosol particles s5um, without mask Aerosol particles s5 um, with mask Fig. 1 Efficacy of surgical face masks in reducing respiratory virus shedding in respiratory droplets and aerosols of symptomatic individuals with coronavirus, influenza virus or rhinovirus infection. a-c Virus copies per sample collected in nasal swab (red), throat swab (blue) and respiratory droplets collected for 30min while not wearing (dark green) or wearing (light green) a surgical face mask, and aerosols collected for 30min while not wearing (brown) or wearing (orange) a face mask, collected from individuals with acute respiratory symptoms who were positive for coronavirus (a), influenza virus (b) and rhinovirus (C), as determined by RT-PCR in any samples. P values for mask intervention as predictor of logo virus copies per sample in an unadjusted univariate Tobit regression model which allowed for censoring at the lower limit of detection of the RT-PCR assay are shown, with significant differences in bold. For nasal swabs and throat swabs, all infected individuals were included (coronavirus, n=17, influenza virus, n=43; rhinovirus, n=54). For respiratory droplets and aerosols, numbers of infected individuals who provided exhaled breath samples while not wearing or wearing a surgical face mask, respectively were: coronavirus (n=10 and 11), influenza virus (n=23 and 28) and rhinovirus (n=36 and 32). A subset of participants provided exhaled breath samples for both mask interventions (coronavirus, n=4; influenza virus, n=8; rhinovirus, n=14). The box plots indicate the median with the interquartile range (lower and upper hinge) and +1.5xinterquartile range from the first and third quartile (lower and upper whiskers). Table 1b Efficacy of surgical face masks in reducing respiratory virus frequency of detection and viral shedding in respiratory droplets and aerosols of symptomatic individuals with coronavirus, influenza virus or rhinovirus infection Droplet particles >5um Aerosol particles 5um (respiratory droplets) were collected by impaction with a 5-um slit inertial Teflon impactor and the remaining fine particles S5um (aerosols) were collected by condensation in buffer. We also demonstrated the efficacy of surgical masks to reduce coronavi- rus detection and viral copies in large respiratory droplets and in aerosols (Table 1b). This has important implications for control of COVID-19, suggesting that surgical face masks could be used by ill people to reduce onward transmission. Among the samples collected without a face mask, we found that the majority of participants with influenza virus and coronavirus infection did not shed detectable virus in respiratory droplets or aerosols, whereas for rhinovirus we detected virus in aerosols in 19 of 34 (56%) participants (compared to 4 of 10 (40%) for influenza and 8 of 23 (35%) for coronavirus). For those who did shed virus in respiratory droplets and aerosols, viral load in both tended to be low (Fig. 1). Given the high collection efficiency of the G-ll (ref." and given that each exhaled breath collection was conducted for 30 min, this might imply that prolonged close contact would be required for transmission to occur, even if transmission was primar- ily via aerosols, as has been described for rhinovirus colds. Our results also indicate that there could be considerable heterogene- ity in contagiousness of individuals with coronavirus and influenza virus infections. The major limitation of our study was the large proportion of participants with undetectable viral shedding in exhaled breath for each of the viruses studied. We could have increased the sam- pling duration beyond 30 min to increase the viral shedding being captured, at the cost of acceptability in some participants. An alternative approach would be to invite participants to perform forced coughs during exhaled breath collection. However, it was the aim of our present study to focus on recovering respiratory Discussion Our results indicate that aerosol transmission is a potential mode of transmission for coronaviruses as well as influenza viruses and rhinoviruses. Published studies detected respiratory viruses such as influenza 2.15 and rhinovirus from exhaled breath, and the detec- tion of SARS-CoV and MERS-CoV from air samples without