Answered step by step
Verified Expert Solution
Question
1 Approved Answer
2 3 5 7 HIM214 REIMBURSEMENT METHODOLOGIES Steps in Utilization Management Utilization Review Below are the basic steps that occur in the prospective, concurrent,
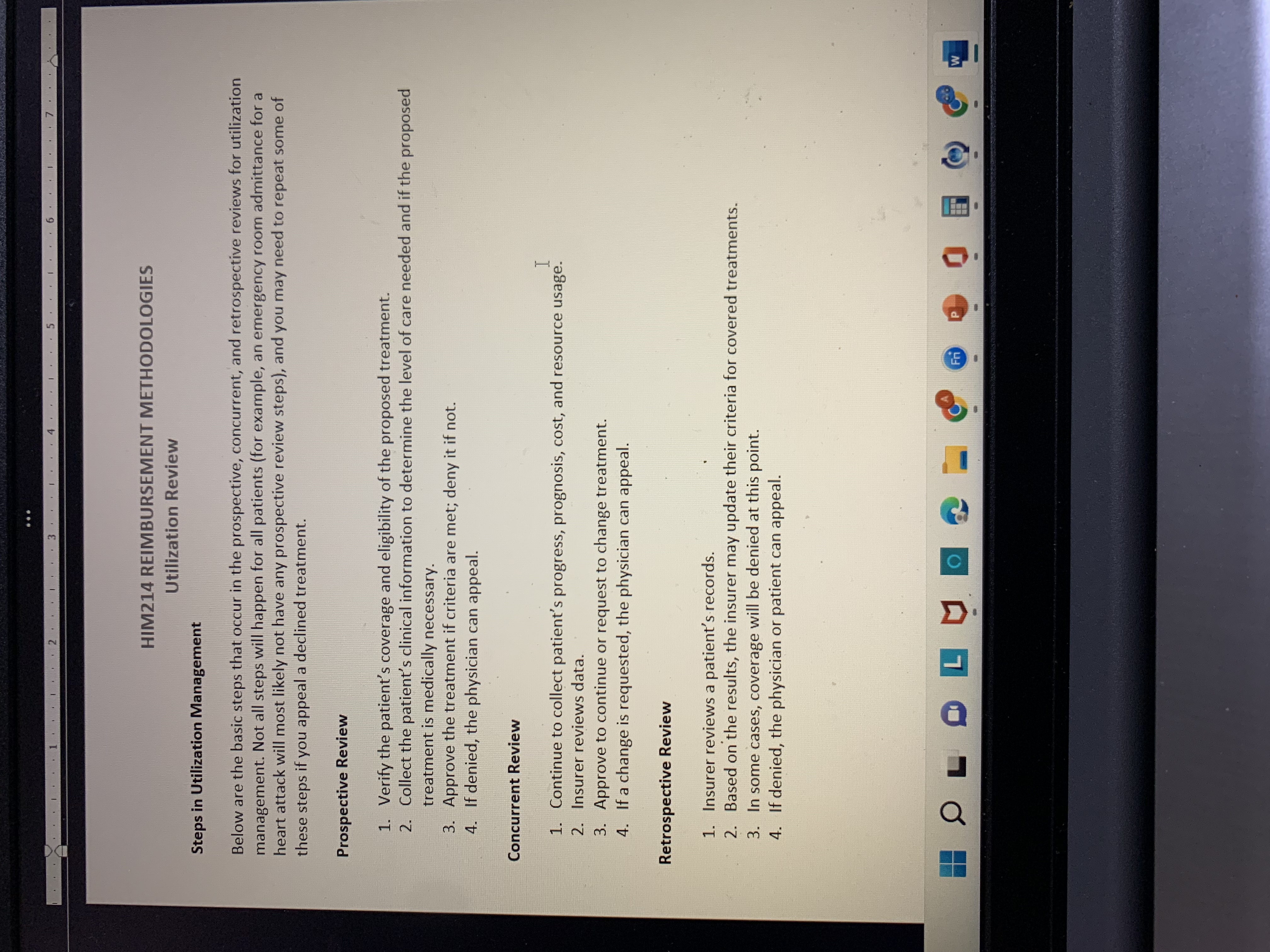
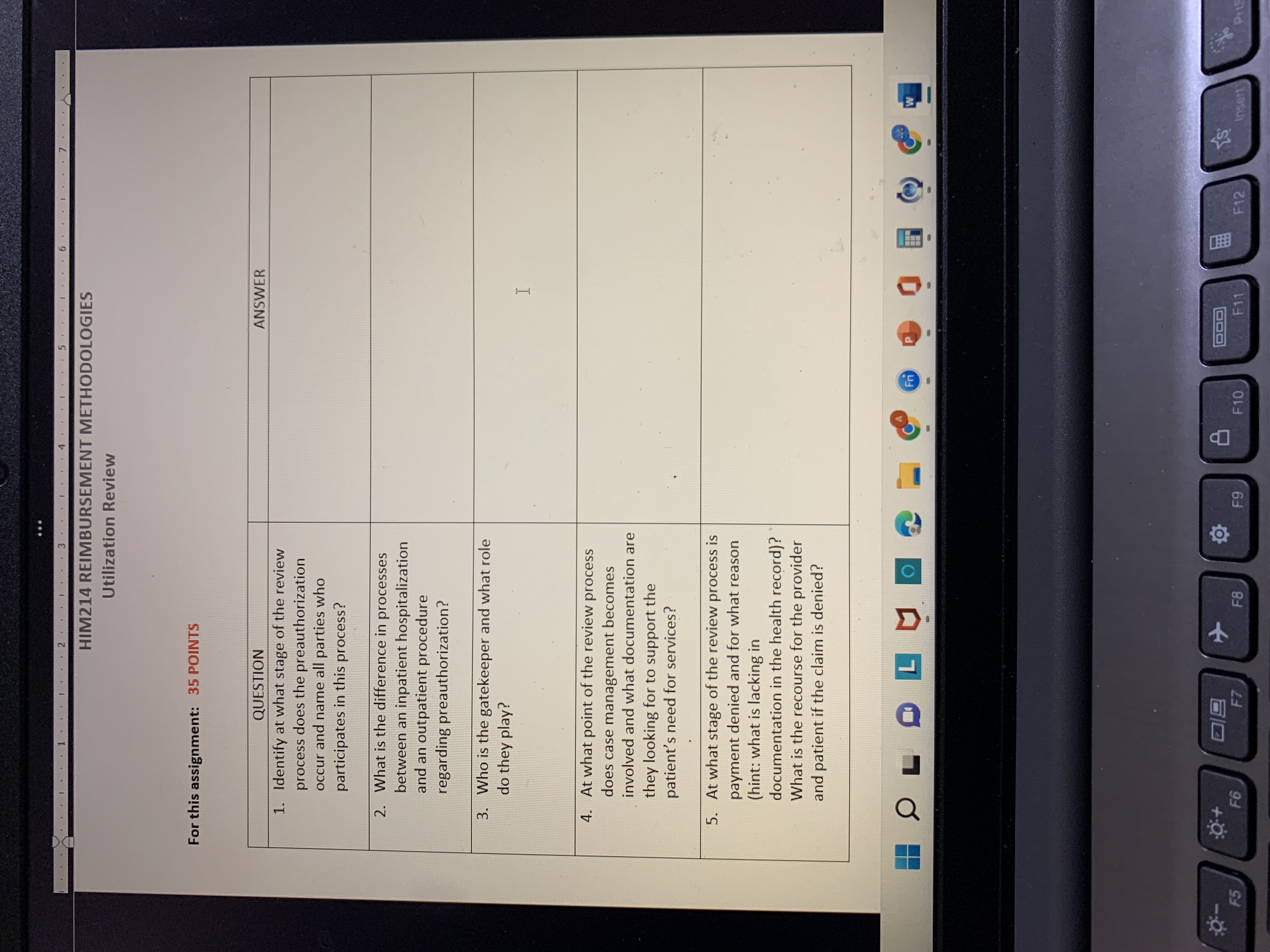
2 3 5 7 HIM214 REIMBURSEMENT METHODOLOGIES Steps in Utilization Management Utilization Review Below are the basic steps that occur in the prospective, concurrent, and retrospective reviews for utilization management. Not all steps will happen for all patients (for example, an emergency room admittance for a heart attack will most likely not have any prospective review steps), and you may need to repeat some of these steps if you appeal a declined treatment. Prospective Review 1. Verify the patient's coverage and eligibility of the proposed treatment. 2. Collect the patient's clinical information to determine the level of care needed and if the proposed treatment is medically necessary. 3. Approve the treatment if criteria are met; deny it if not. 4. If denied, the physician can appeal. Concurrent Review I 1. Continue to collect patient's progress, prognosis, cost, and resource usage. 2. Insurer reviews data. 3. Approve to continue or request to change treatment. 4. If a change is requested, the physician can appeal. Retrospective Review 1. Insurer reviews a patient's records. 2. Based on the results, the insurer may update their criteria for covered treatments. 3. In some cases, coverage will be denied at this point. 4. If denied, the physician or patient can appeal. L = Fri W ..2 3 . . 5 . 7 HIM214 REIMBURSEMENT METHODOLOGIES Utilization Review For this assignment: 35 POINTS QUESTION 1. Identify at what stage of the review process does the preauthorization occur and name all parties who participates in this process? 2. What is the difference in processes between an inpatient hospitalization and an outpatient procedure regarding preauthorization? 3. Who is the gatekeeper and what role do they play? 4. At what point of the review process does case management becomes involved and what documentation are they looking for to support the patient's need for services? 5. At what stage of the review process is payment denied and for what reason (hint: what is lacking in documentation in the health record)? What is the recourse for the provider and patient if the claim is denied? LOFY - B F5 F6 F7 + ANSWER I E Fr W F8 F9 F10 F11 HEE S F12 Insert Pris
Step by Step Solution
There are 3 Steps involved in it
Step: 1

Get Instant Access to Expert-Tailored Solutions
See step-by-step solutions with expert insights and AI powered tools for academic success
Step: 2

Step: 3

Ace Your Homework with AI
Get the answers you need in no time with our AI-driven, step-by-step assistance
Get Started