Question: Answer this correctly Exam Content The patient is a 55 year old female who presented at the dermatclogist with large erythematous [Q1] (itchy, red, painful)
Answer this correctly
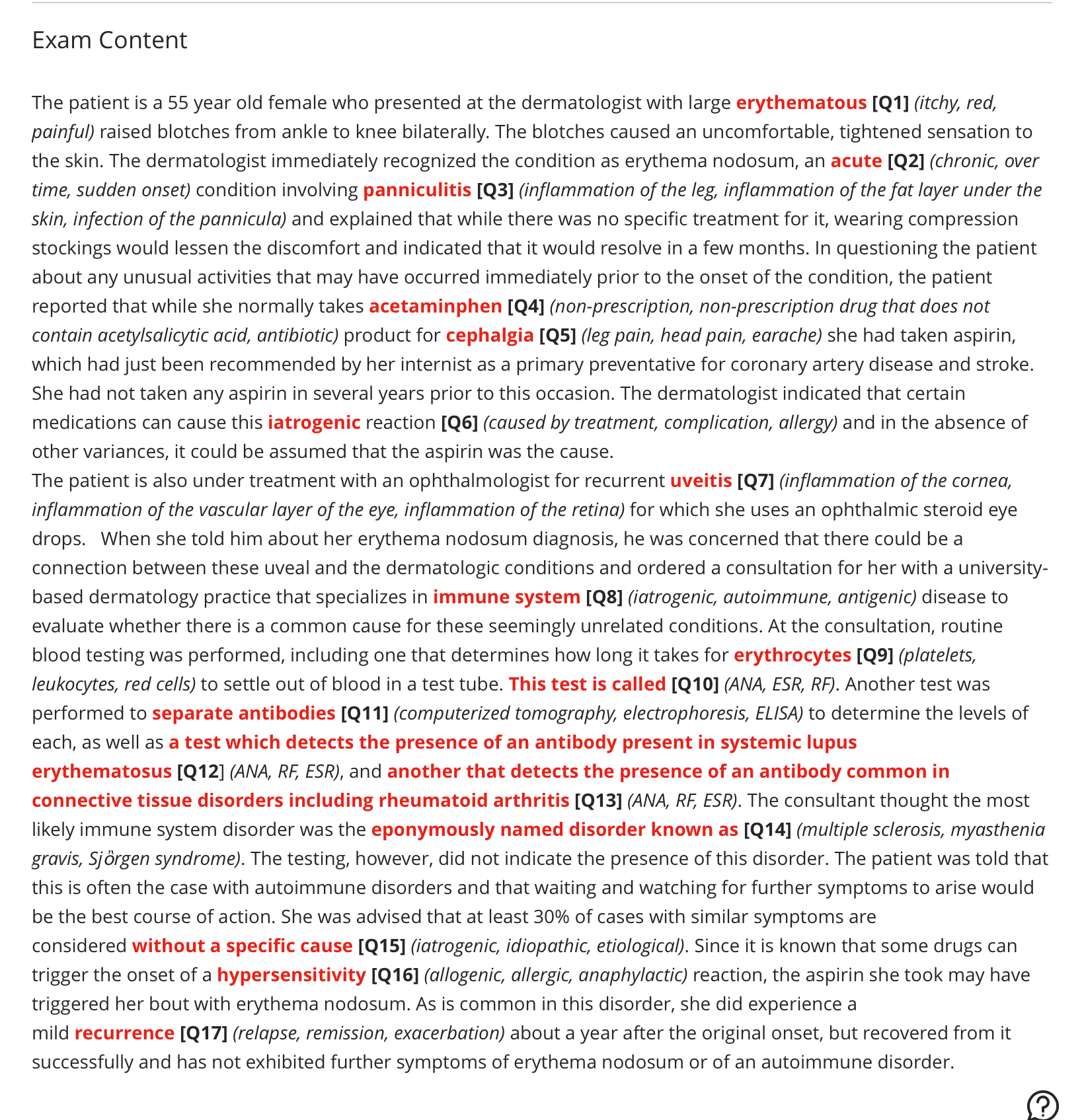
Exam Content The patient is a 55 year old female who presented at the dermatclogist with large erythematous [Q1] (itchy, red, painful) raised blotches from ankle to knee bilaterally. The blotches caused an uncomfortable, tightened sensation to the skin. The dermatologist immediately recognized the condition as erythema nodosum, an acute [Q2] (chronic, over time, sudden onset) condition involving panniculitis [Q3] (inflammation of the leg, inflammation of the fat layer under the skin, infection of the pannicula) and explained that while there was no specific treatment for it, wearing compression stockings would lessen the discomfort and indicated that it would resolve in a few months. In questioning the patient about any unusual activities that may have occurred immediately prior to the onset of the condition, the patient reported that while she normally takes acetaminphen [Q4] (non-prescription, hon-prescription drug that does not contain acetylsalicytic acid, antibiotic) product for cephalgia [Q5] (leg pain, head pain, earache) she had taken aspirin, which had just been recommended by her internist as a primary preventative for coronary artery disease and stroke. She had not taken any aspirin in several years prior to this occasion. The dermatologist indicated that certain medications can cause this iatrogenic reaction [Q6] (caused by treatment, complication, allergy) and in the absence of other variances, it could be assumed that the aspirin was the cause. The patient is also under treatment with an ophthalmologist for recurrent uveitis [Q7] (inflammation of the cornea, inflammation of the vascular layer of the eye, inflammation of the retina) for which she uses an ophthalmic steroid eye drops. When she told him about her erythema nodosum diagnosis, he was concerned that there could be a connection between these uveal and the dermatologic conditions and ordered a consultation for her with a university- based dermatology practice that specializes in immune system [Q8] (iatrogenic, autoimmune, antigenic) disease to evaluate whether there is a common cause for these seemingly unrelated conditions. At the consultation, routine blood testing was performed, including one that determines how long it takes for erythrocytes [Q9] (platelets, leukocytes, red cells) to settle out of blood in a test tube. This test is called [Q10] (ANA, ESR, RF). Another test was performed to separate antibodies [Q11] (computerized tomography, electropharesis, ELISA) to determine the levels of each, as well as a test which detects the presence of an antibody present in systemic lupus erythematosus [Q12] (ANA, RF, ESR), and another that detects the presence of an antibody common in connective tissue disorders including rheumatoid arthritis [Q13] (ANA, RF, ESR). The consultant thought the most likely immune system disorder was the eponymously named disorder known as [Q14] (multiple sclerosis, myasthenia gravis, Sjorgen syndrome). The testing, however, did not indicate the presence of this disorder. The patient was told that this is often the case with autoimmune disorders and that waiting and watching for further symptoms to arise would be the best course of action. She was advised that at least 30% of cases with similar symptoms are considered without a specific cause [Q15] (iatrogenic, idiopathic, etiological). Since it is known that some drugs can trigger the onset of a hypersensitivity [Q16] (allogenic, allergic, anaphylactic) reaction, the aspirin she took may have triggered her bout with erythema nodosum. As is common in this disorder, she did experience a mild recurrence [Q17] (relapse, remission, exacerbation) about a year after the original onset, but recovered from it successfully and has not exhibited further symptoms of erythema nodosum or of an autoimmune disorder. @