Answered step by step
Verified Expert Solution
Question
1 Approved Answer
can someone help me fill out a E&M audit please i need help filling out an evaluation and managment audit form. I included the E&M
can someone help me fill out a E&M audit please 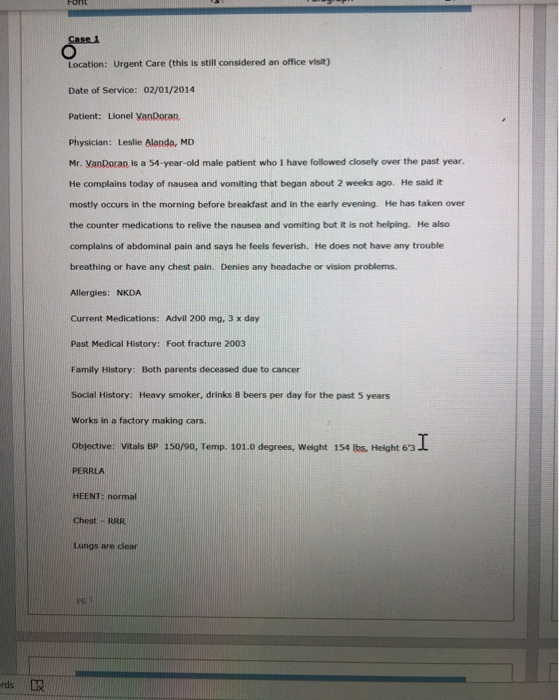
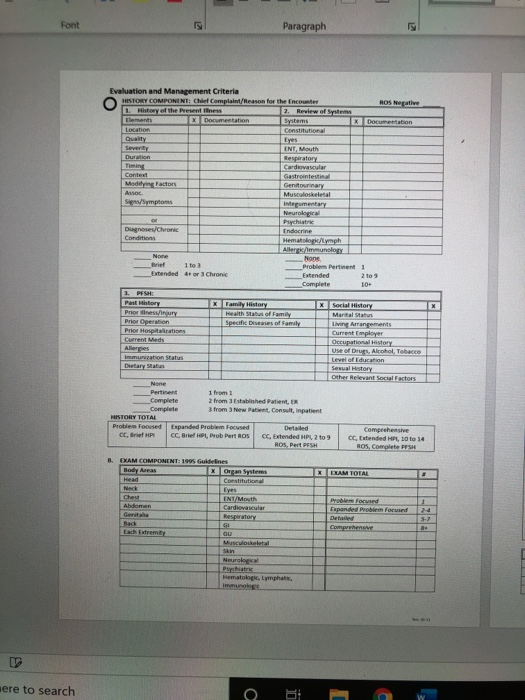
i need help filling out an evaluation and managment audit form. I included the E&M form.
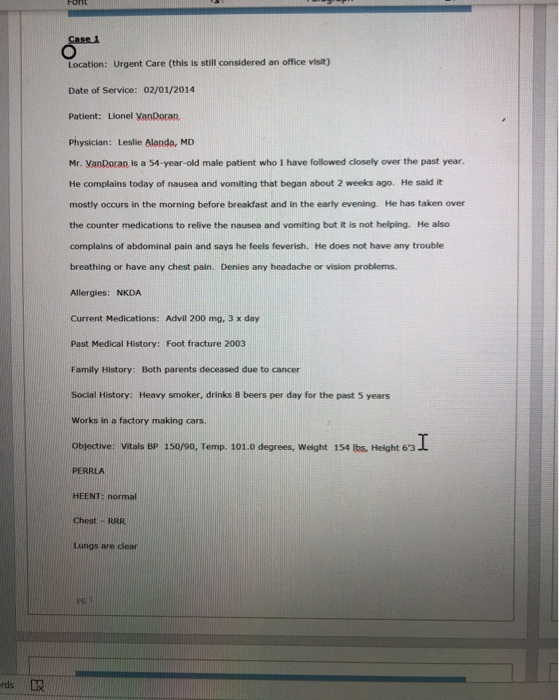
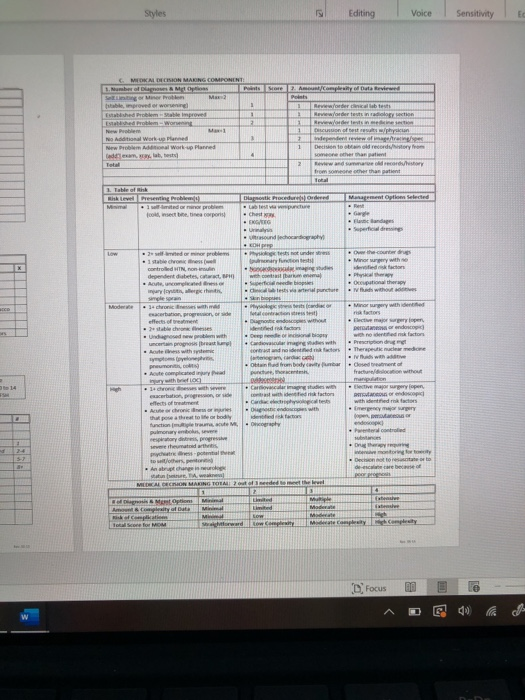
Font Case 1 Location: Urgent Care (this is still considered an office visit) Date of Service: 02/01/2014 Patient: Lionel VanDoran Physician: Leslie Alanda, MD Mr. VanDocan is a 54-year-old male patient who I have followed closely over the past year. He complains today of nausea and vomiting that began about 2 weeks ago. He said it mostly occurs in the morning before breakfast and in the early evening. He has taken over the counter medications to relive the nausea and vomiting but it is not helping. He also complains of abdominal pain and says he feels feverish. He does not have any trouble breathing or have any chest pain. Denies any headache or vision problems. Allergies: NKDA Current Medications: Advil 200 mg, 3 x day Past Medical History: Foot fracture 2003 Family History: Both parents deceased due to cancer Social History: Heavy smoker, drinks & beers per day for the past 5 years Works in a factory making cars. Objective: Vitals BP 150/90, Temp. 101.0 degrees, Weight 154 lbs, Height 6'3 Height 63 I PERRLA HEENT: normal Chest - RRR Lungs are dear PE rds LX Abdomen - tenderness in the upper abdomen No rashes on skin No lymphadenopathy Assessment and Plan 54-year-old patient with 2-week history of nausea and vomiting. Blood work ordered to rule out any bacterial infections. Abdominal x-ray ordered to rule out appendicitis, also need to consider liver disease due to the patient's history of alcohol intake. Give patient an IV of hydration solution and some Tylenol for the fever. Have patient follow up with their primary care provider to review test results. Font Paragraph X Evaluation and Management Criteria HISTORY COMPONENT Chef Complaint/Reason for the Encounter ROS Negative 1. History of the Presentes 2. Review of Stems Thements x Documentation Systems Documentation Location Constitutional Duality INT, Mouth Duration Respiratory Cardiovascular Contest Gastrointestinal Madilying Factor Genitourinary Anso Musculoskeletal Signs/Symptoms Integumentary Neurological Psychiatric Dugnases/Chronic Endocrine Conditions Hematolog/Lymph Allerg/Immunology None None brief 1to3 Problem pertinent 1 Extended 4+ or Chronic Extended 219 Complete 10+ 2. PESHE Pastory x Family History x Social History Priorines injury Health status of Family Marital Status Prior Operation Specific Diseases of Family Living Arrangements Prior Hospitations Current Employer Current Meds Occupational History Allergies Use of Druts, Alcohol, Tobacco Immunication Status Level of Education Dietary Status Sewal History Other Relevant Social Factors None Pertinent 1 from Complete 2 from Established Patient, ER Complete 3 from New Patient Consult, inpatient HISTORY TOTAL Problem Focused Expanded Problem focused Detailed Comprehensive CC, Brief HP: CC. Brief H, Prob Port ROS CC, Extended HPL 2 to 9 OC, Extended HP, 10 to 14 ROS, Pert PESH ROS, Complete X EXAM TOLAL 1 B. EXAM COMPONENT: 1995 Guidelines Body Areas xOrgan Systems Head Constitutional Neck Chest ENT/Mouth Abdomen Cardiovascular Respiratory Back GI GU Musculoskeletal Skin Problem forved Papanded Problem forvard Detailed Comprehensive Hematolog, Lymphate, Immunologs here to search O Styles Editing Voice Sensitivity e Step by Step Solution
There are 3 Steps involved in it
Step: 1

Get Instant Access to Expert-Tailored Solutions
See step-by-step solutions with expert insights and AI powered tools for academic success
Step: 2

Step: 3

Ace Your Homework with AI
Get the answers you need in no time with our AI-driven, step-by-step assistance
Get Started