Help! I need help to answer this case study. Could you please help me with the questions and each section. The first two question is not really relevant because that is self evident. However question 4 to 16 I am really struggling. Could someone help me. Please any help with any section. Or just a place to start please!
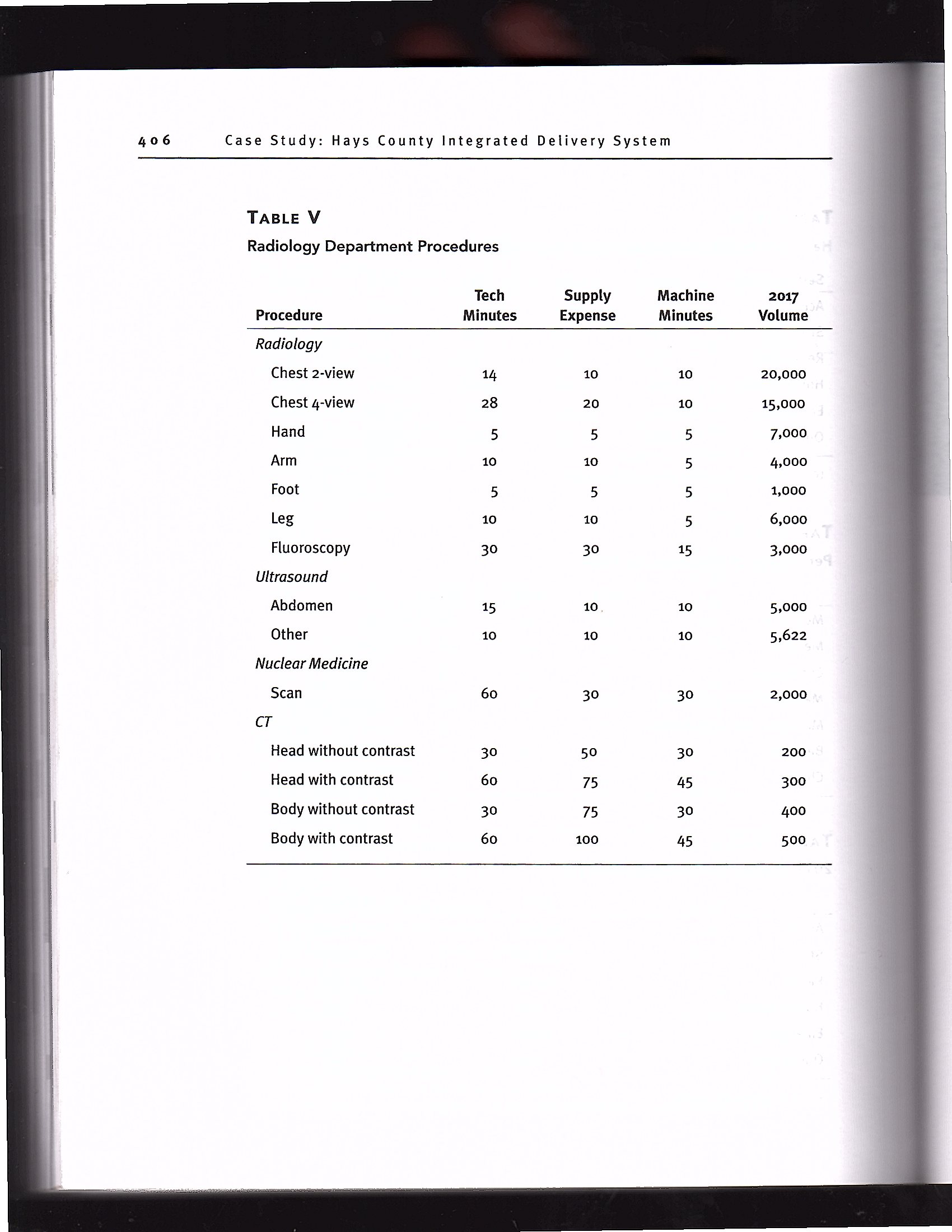
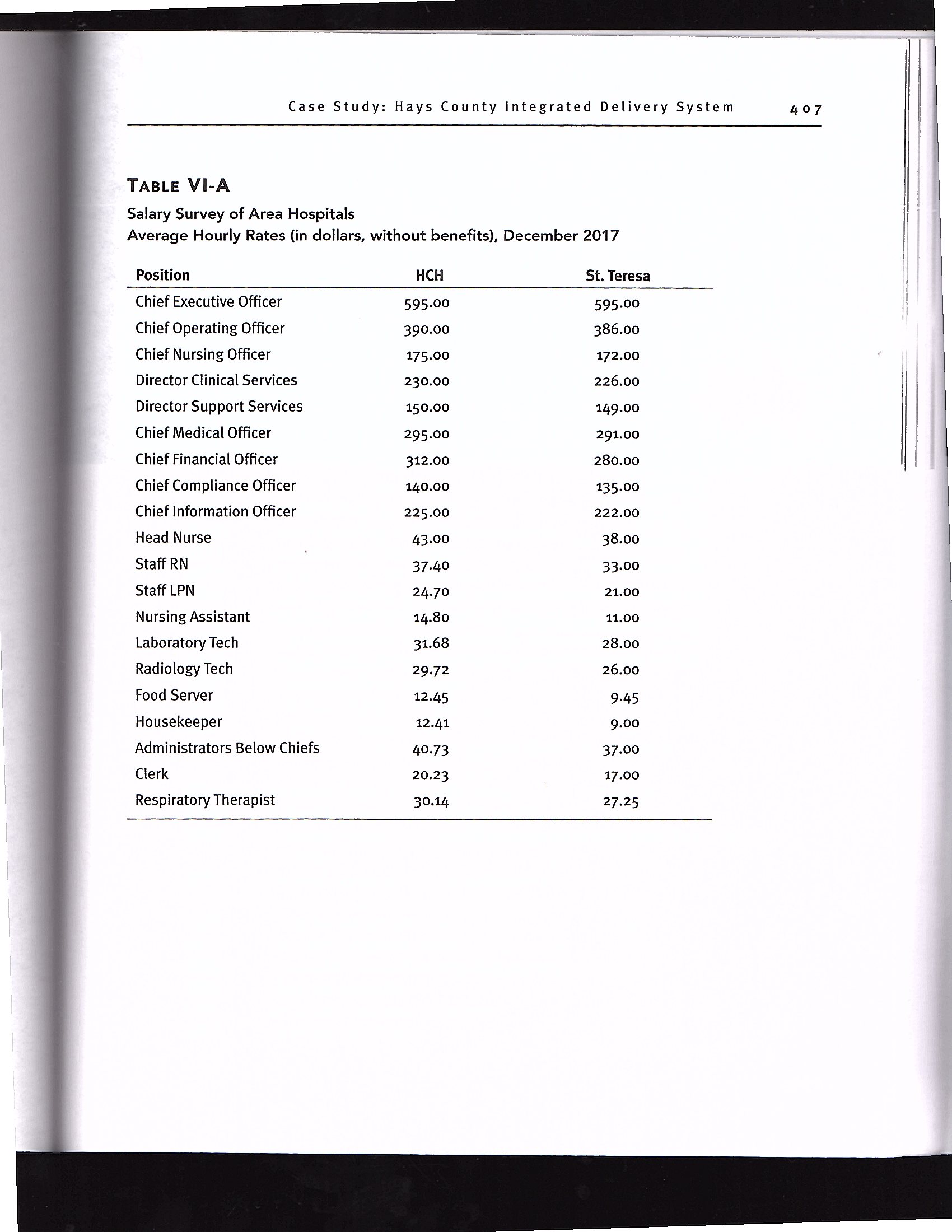
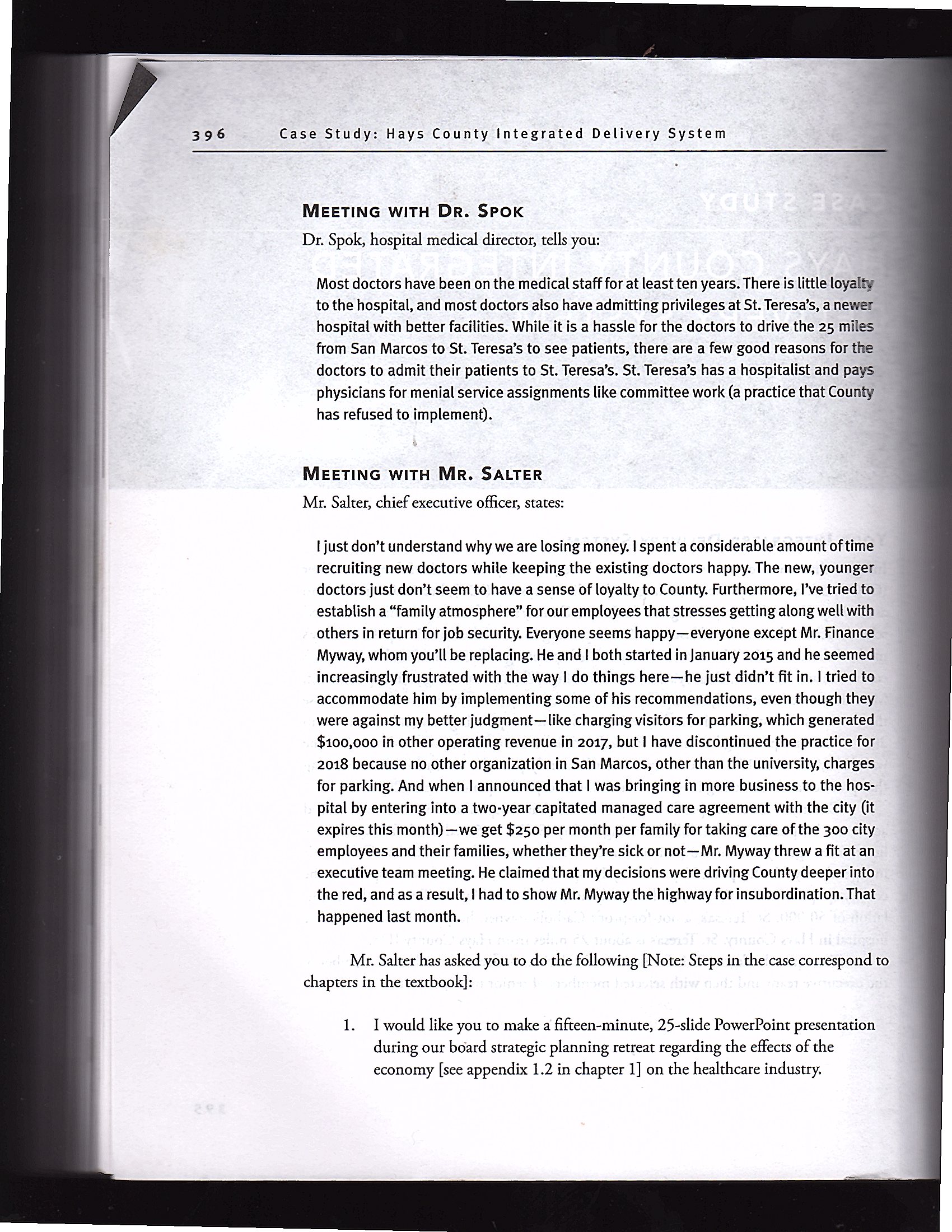
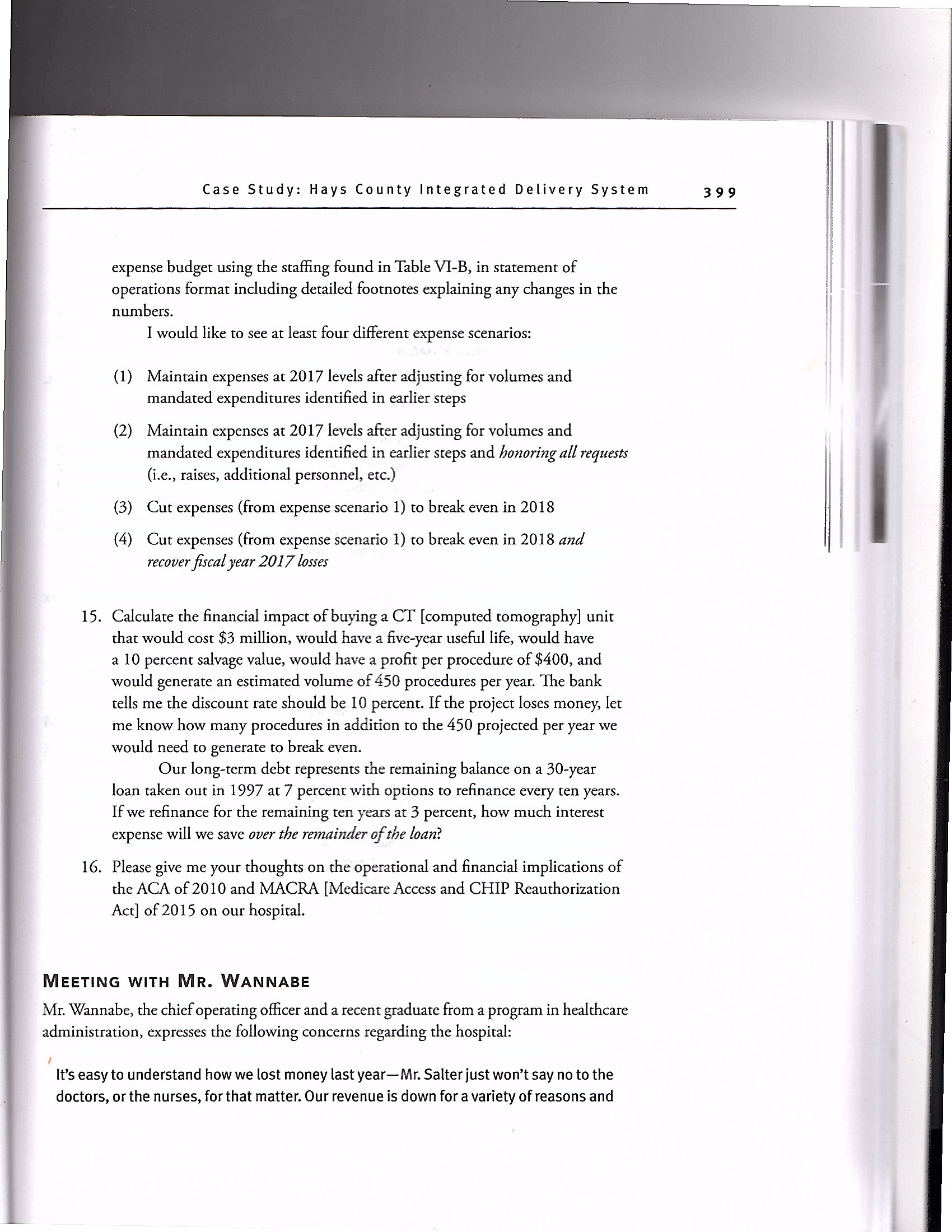
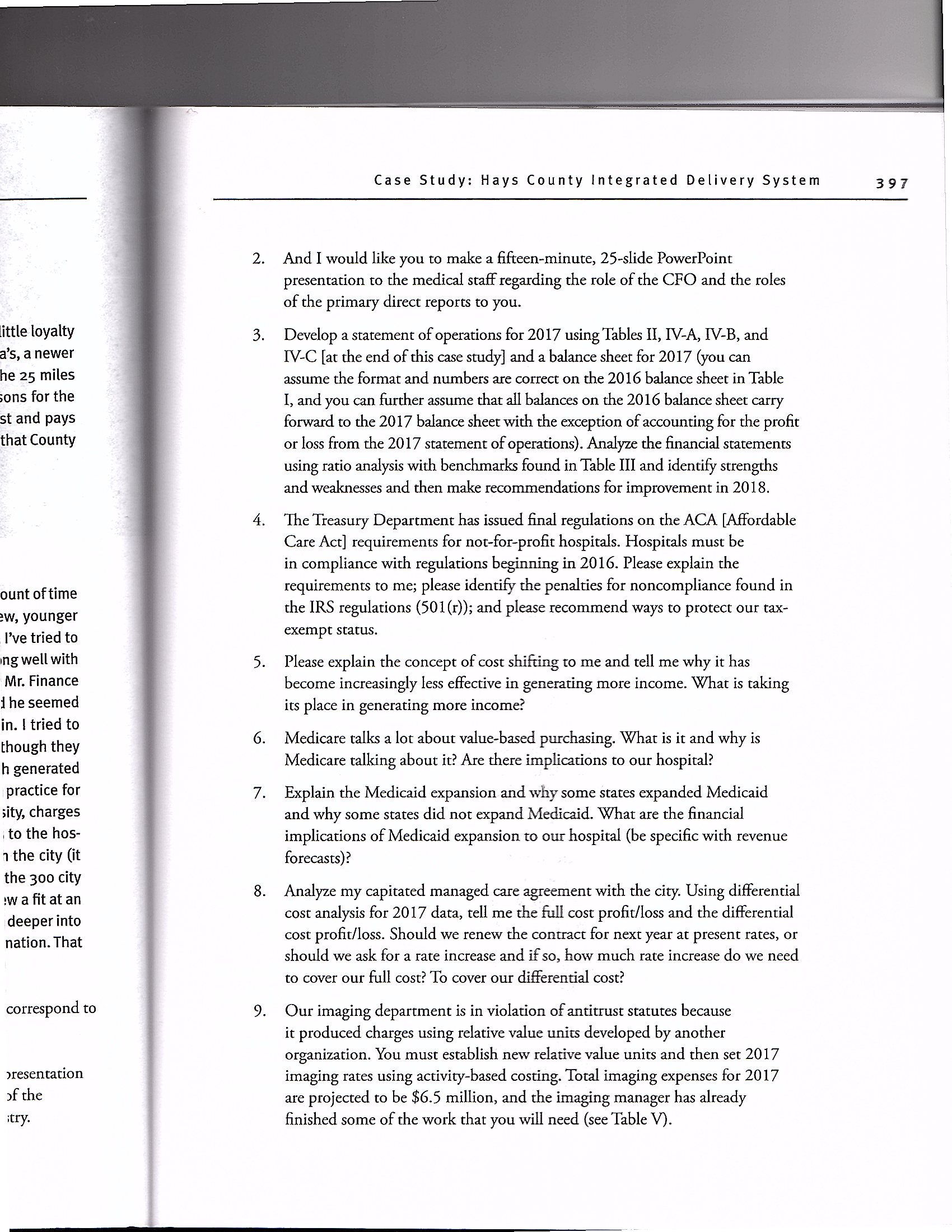
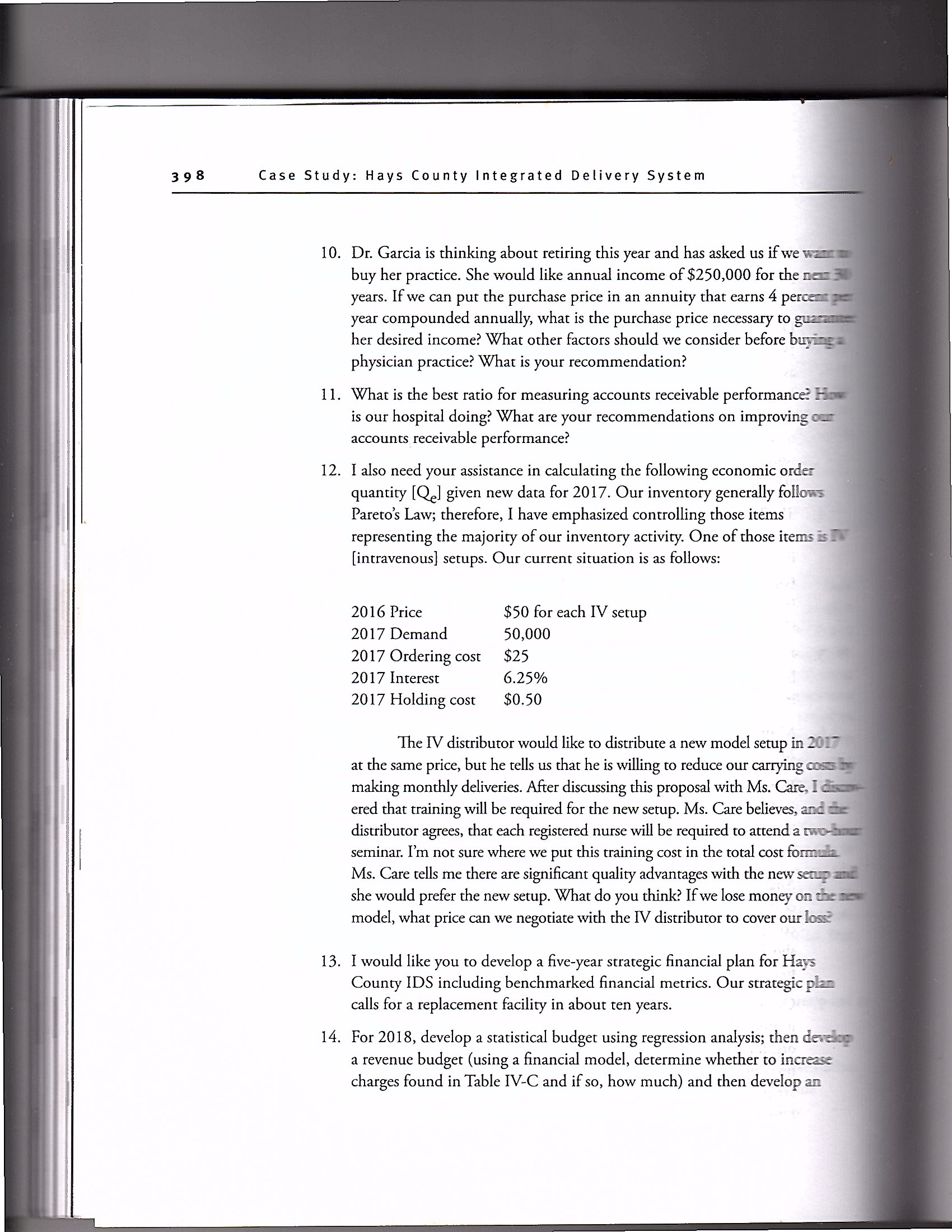
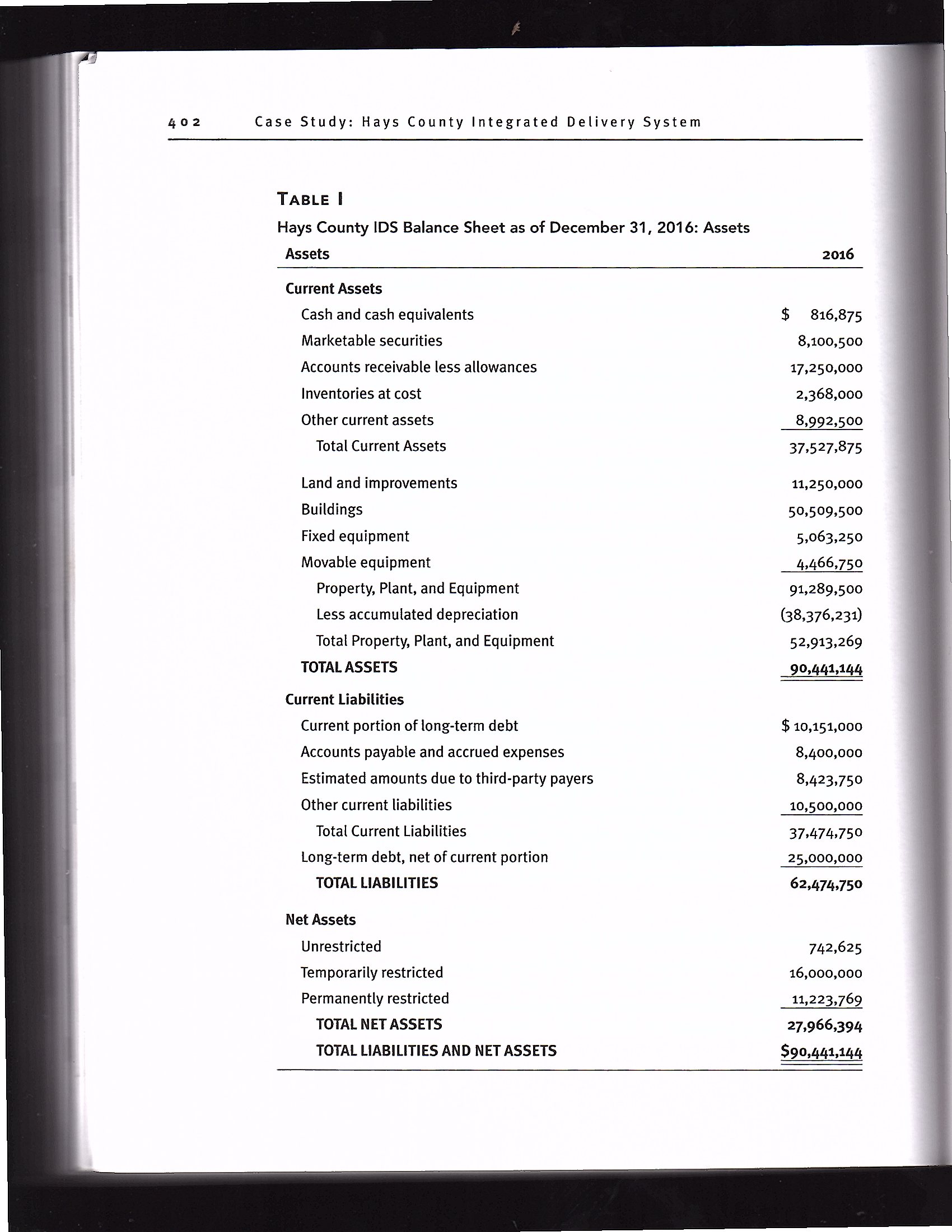
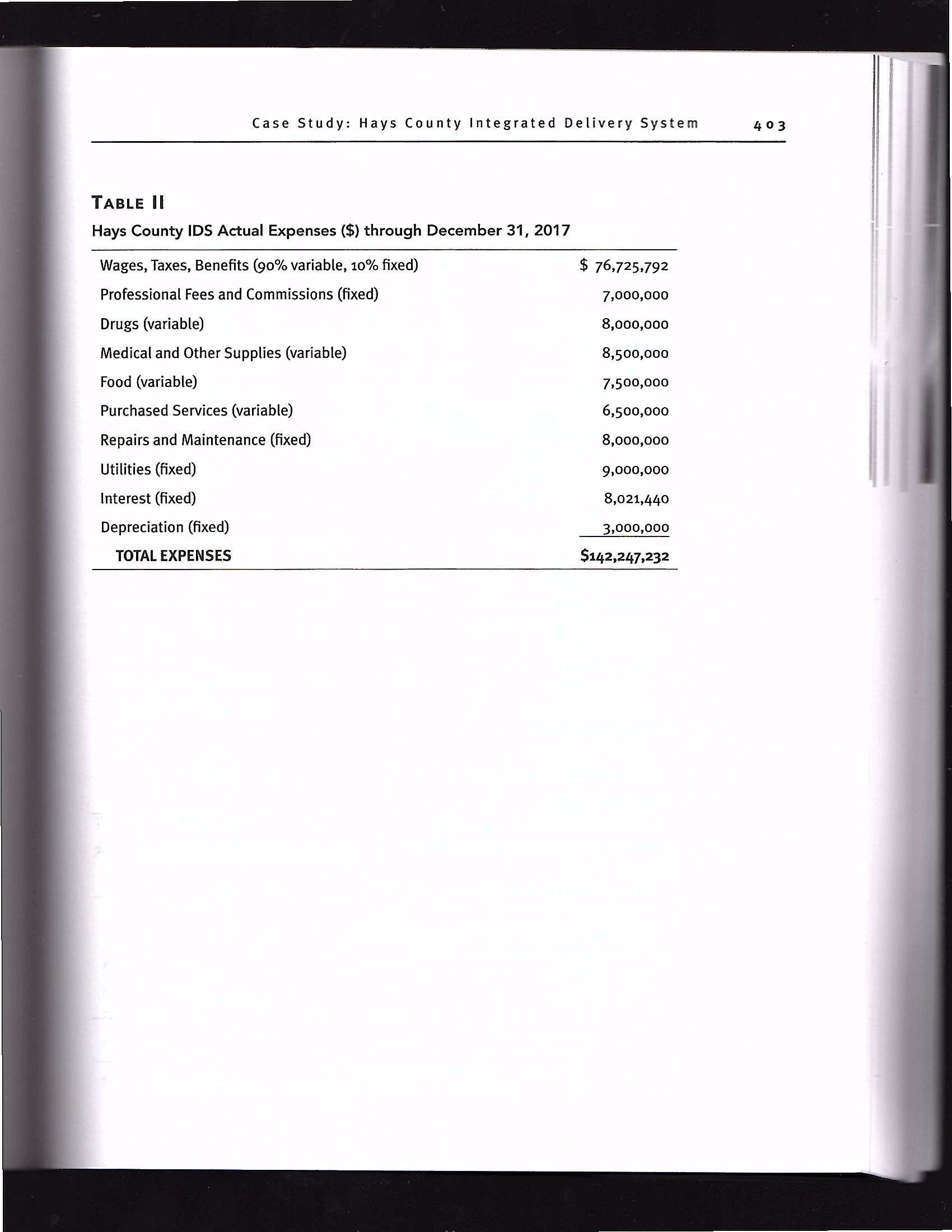
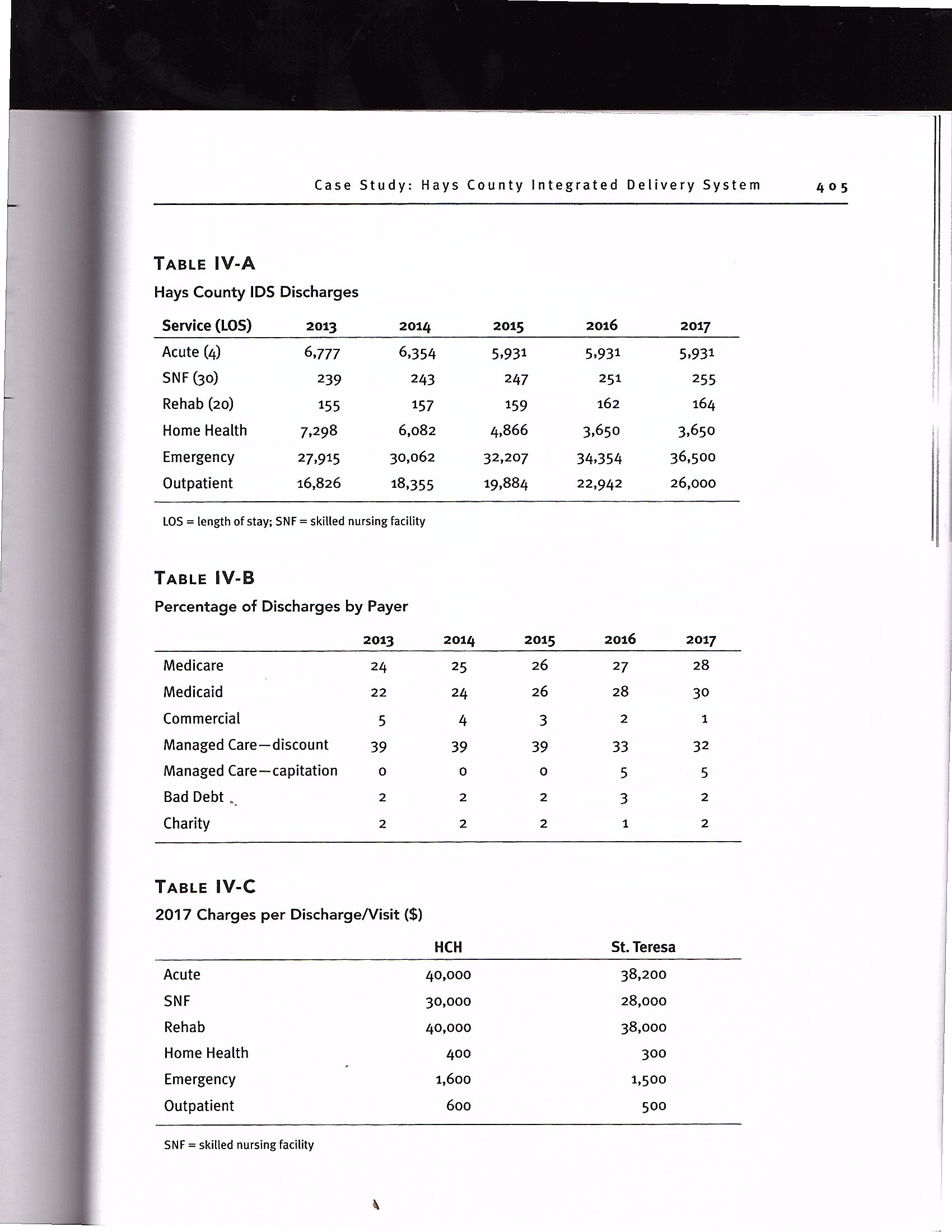
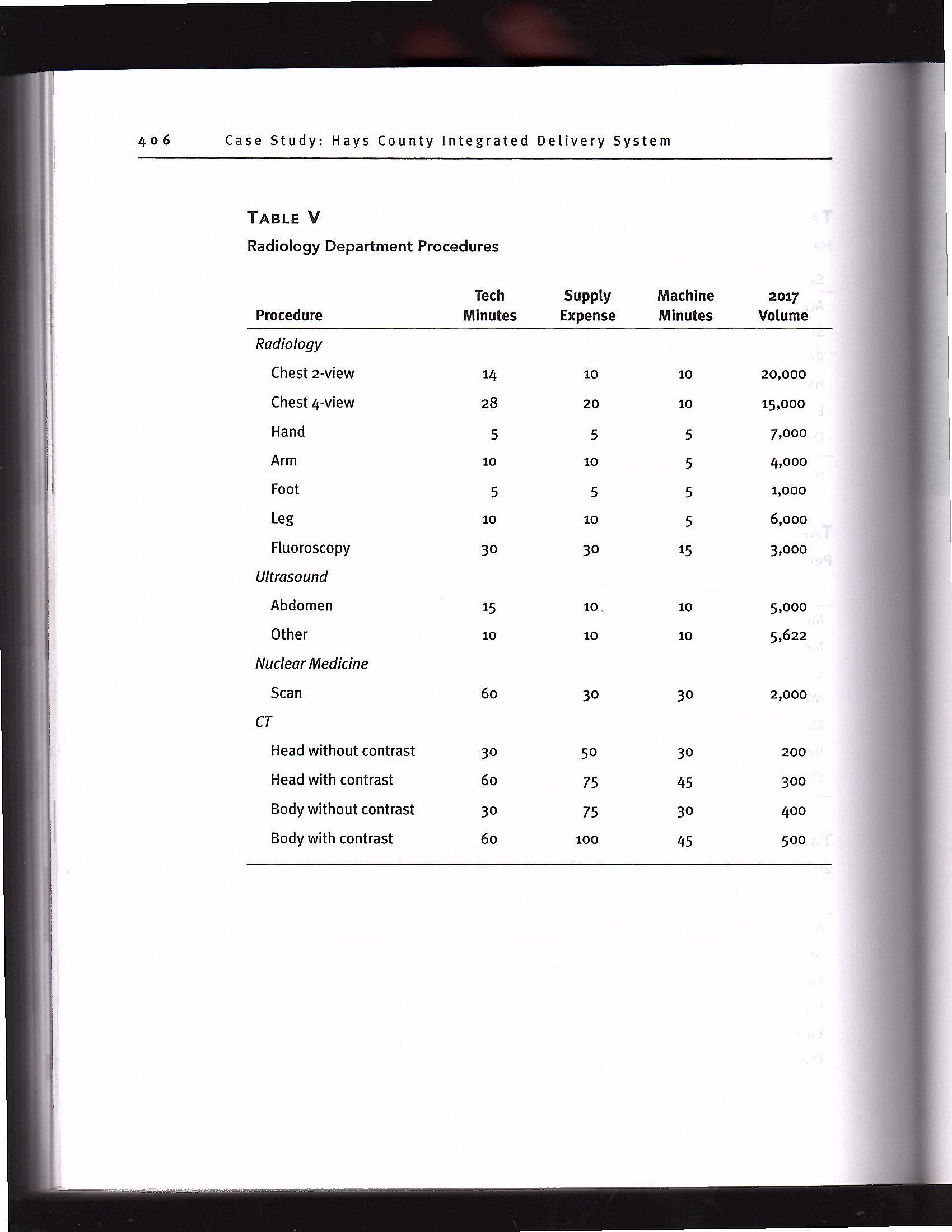
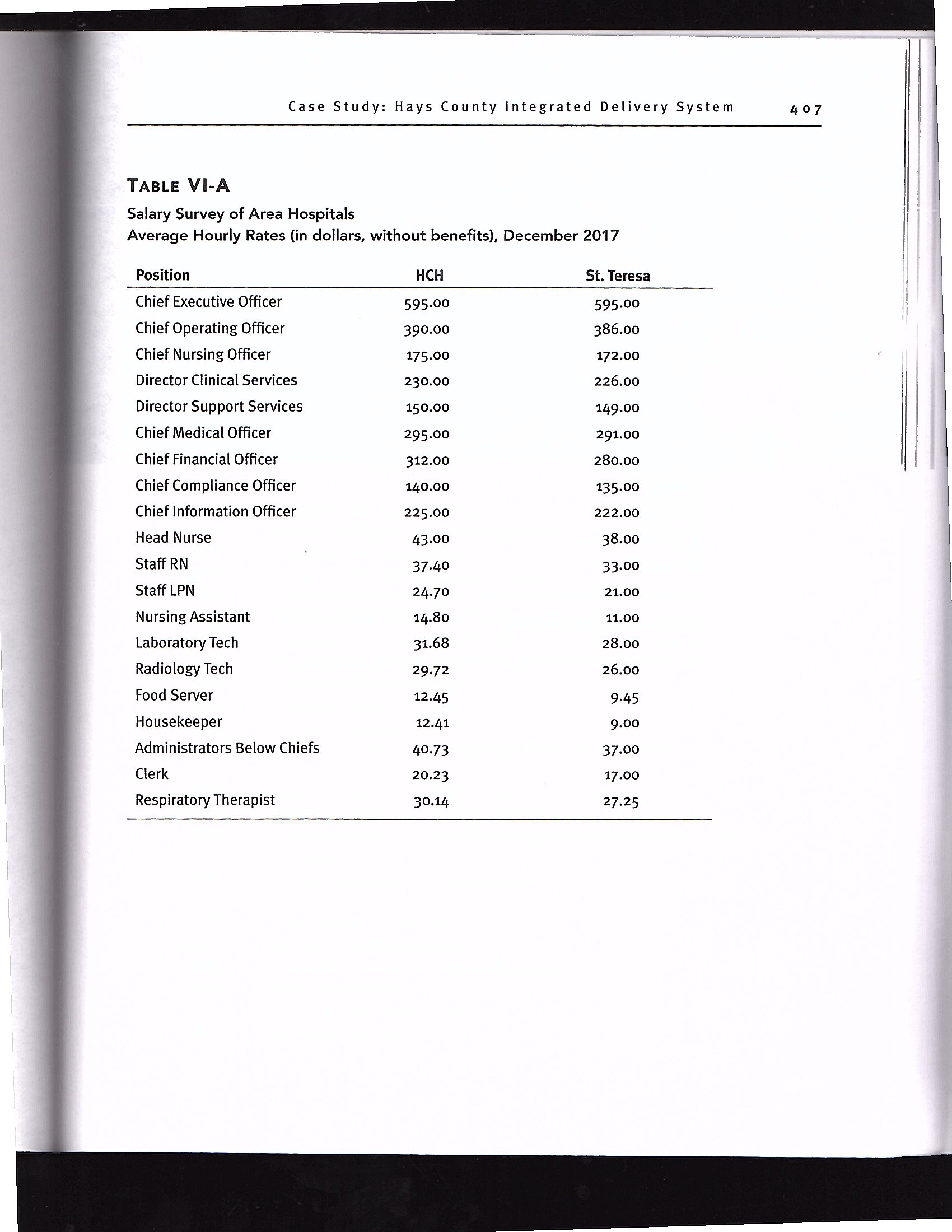
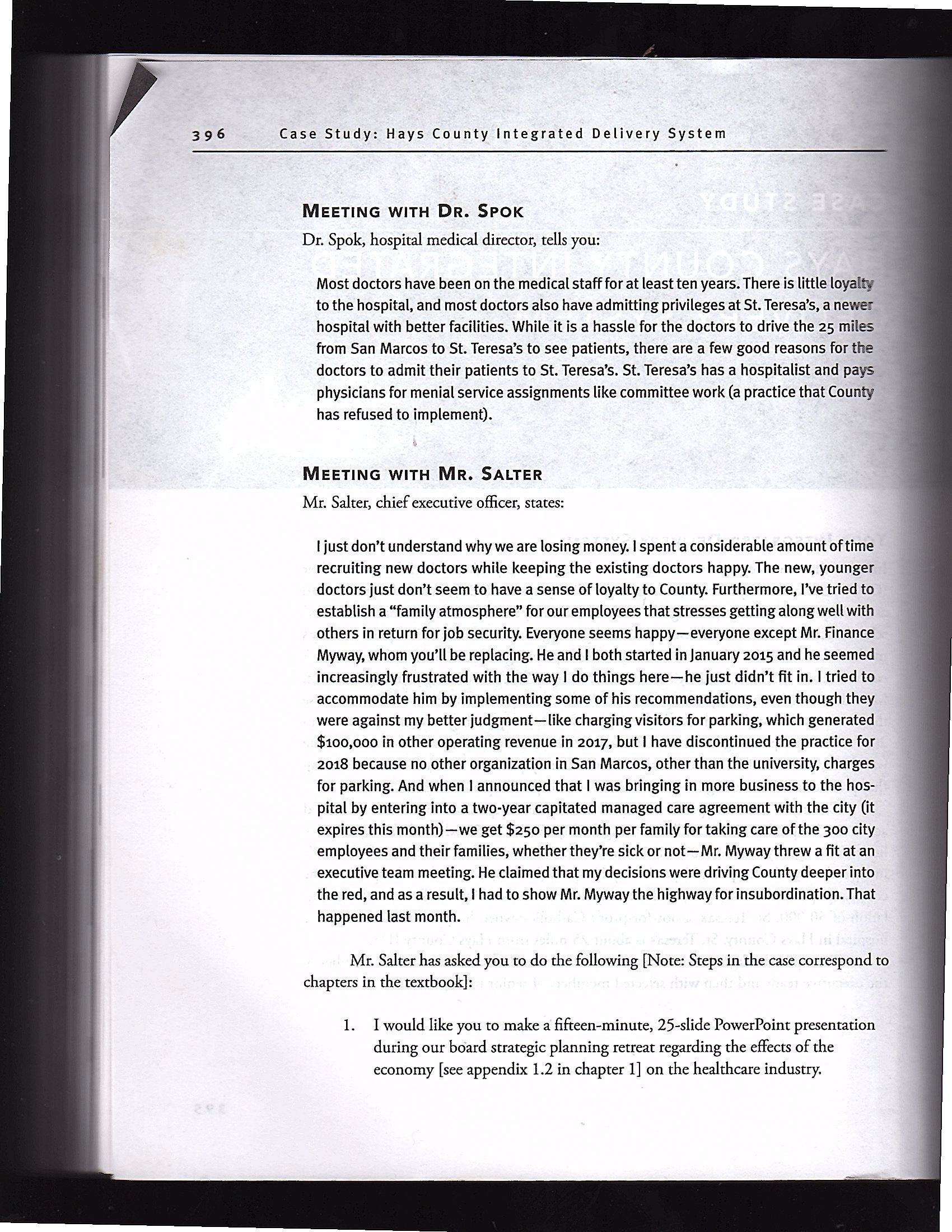
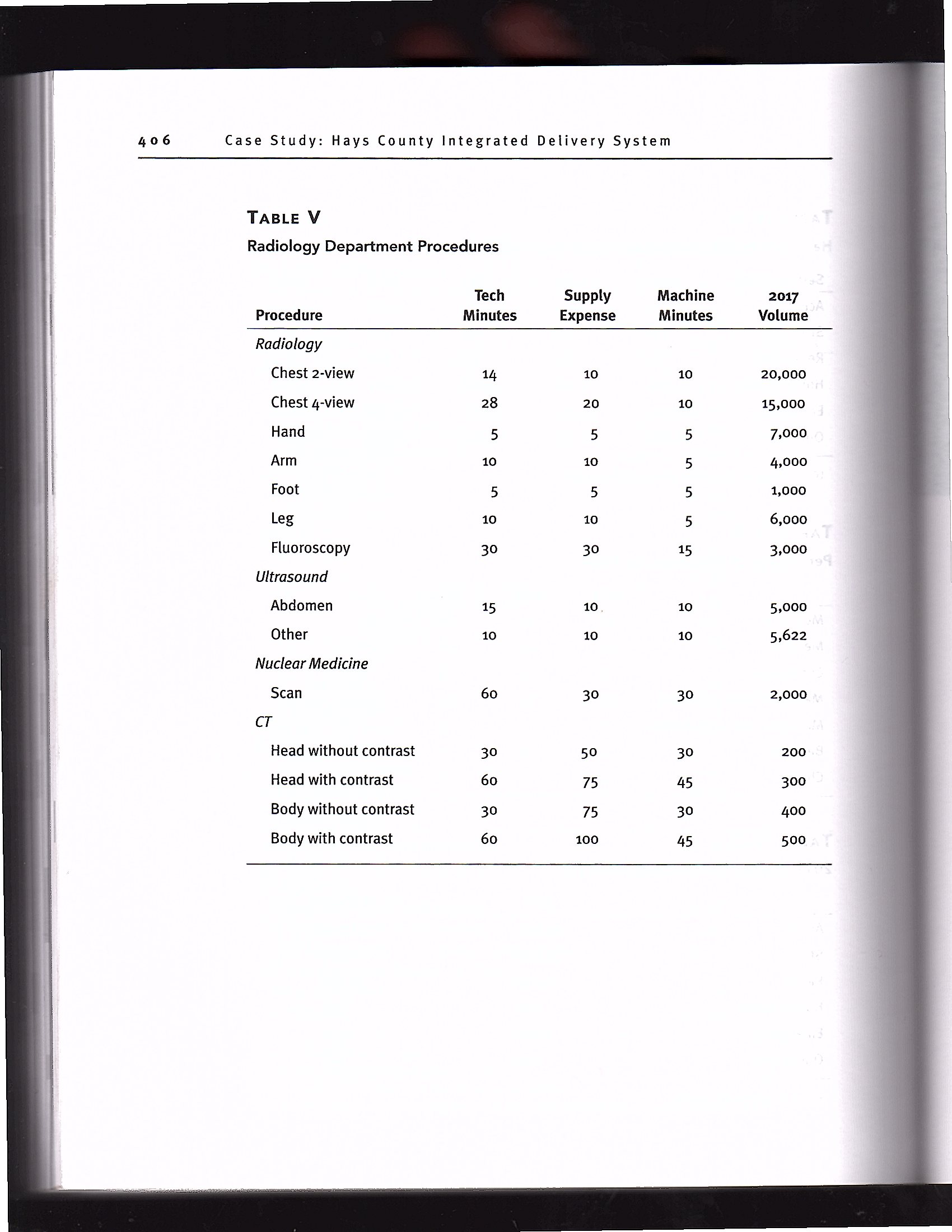
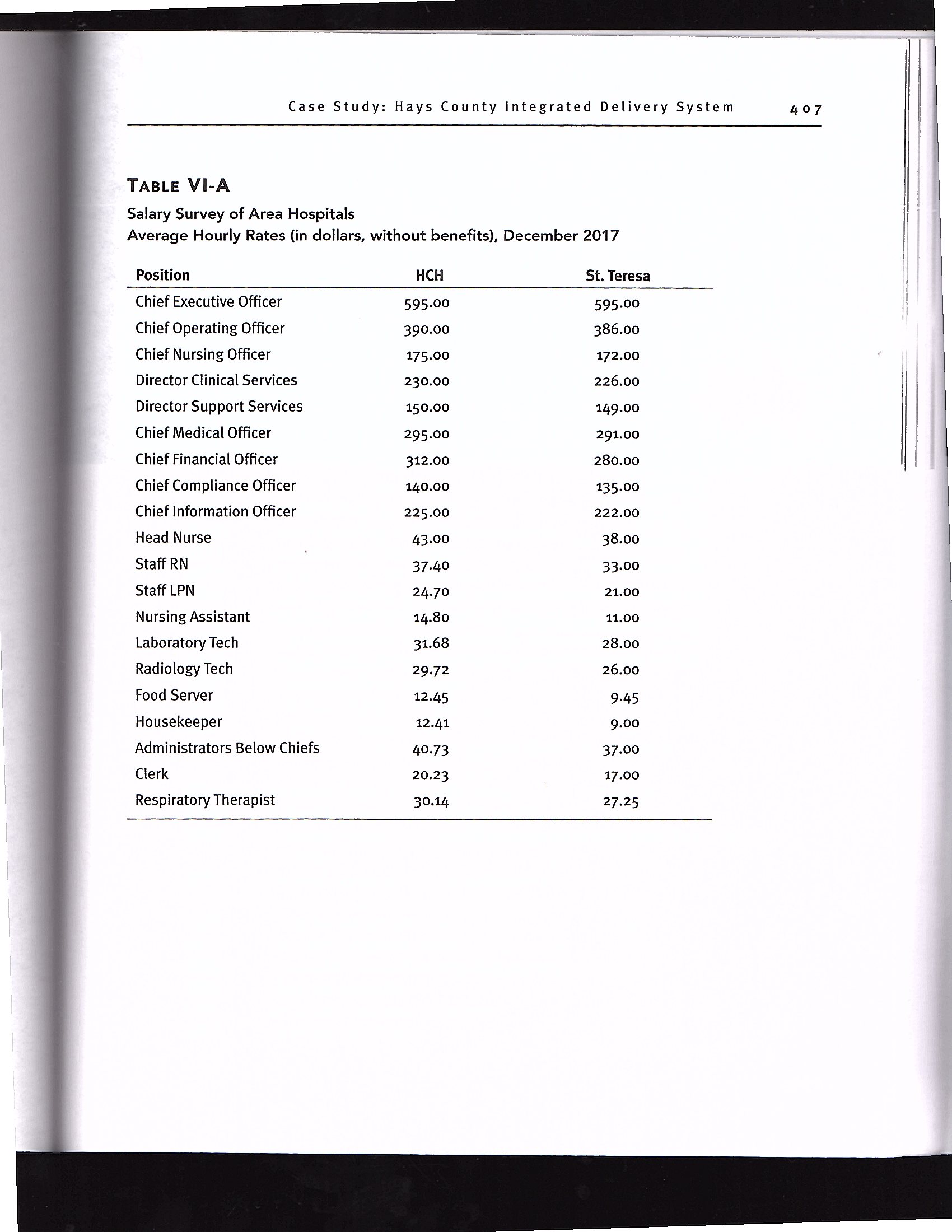
Case Study: Hays County Integrated Delivery System TABLE I Hays County IDS Balance Sheet as of December 31, 2016: Assets Assets 2016 Current Assets Cash and cash equivalents $ 816,875 Marketable securities 8,100,500 Accounts receivable less allowances 17,250,000 Inventories at cost 2,368,000 Other current assets 8,992,500 Total Current Assets 37.527375 Land and improvements 11,250,000 Buildings 50,509,500 Fixed equipment 5,063,250 Movable equipment 4,466,750 Property, Plant, and Equipment 91,289,500 Less accumulated depreciation (38376231) Total Property, Plant, and Equipment 52,913,269 TOTAL ASSETS 90,441,144 Current Liabilities Current portion of long-term debt $ 10,151,000 Accounts payabie and accrued expenses 8,400,000 Estimated amounts due to third-party payers 8,423,750 Other current liabilities 10,500,000 Total Current Liabilities 37,474,750 Long-term debt, net of current portion 25,000,000 TOTAL LIABILITIES 62,474,750 Net Assets Unrestricted 742,625 Temporarily restricted 16,000,000 Permanently restricted 11,223,769 TOTAL NET ASSETS 27.966394 TOTAL LIABILITIES AND NET ASSETS $90,441,144 Case Study: Hays County Integrated Delivery System 403 TABLE II Hays County IDS Actual Expenses ($) through December 31, 2017 Wages, Taxes, Benefits (90% variable, 10% fixed) $ 76,725,792 Professional Fees and Commissions (fixed) 7,000,000 Drugs (variable) 8,000,000 Medical and Other Supplies (variable) 8,500,000 Food (variable) 7,500,000 Purchased Services (variable) 6,500,000 Repairs and Maintenance (fixed) 8,000,000 Utilities (fixed) 9,000,000 Interest (fixed) 8,021,440 Depreciation (fixed) 3,000,000 TOTAL EXPENSES $142,247,232- an =ca; ' 'f'ria Case Study: Hays County Integrated Delivery System TABLE lV-A Hays County IDS Discharges Service (L05) 2013 2014 2015 2016 2017 Acute (4) 6.777 6,354 5.931 5-931 5931 SNF (30) 239 243 247 251 255 Rehab (20) 155 157 159 162 164 Home Health 7,298 6,082 4,866 3,650 3,650 Emergency 27,915 30,062 32,207 34,354 36,500 Outpatient 16,826 18,355 19,884 22,942 26,000 L05 = length ofstay: SNF: skilled nursing facility TABLE IV-B Percentage of Discharges by Payer 2013 2014 2015 2016 2017 Medicare 24 25 26 27 28 Medicaid 22 24 26 28 30 Commercial 5 4 3 2 1 Managed Carediscount 39 39 39 33 32 Managed Carecapitation 0 0 0 5 5 Bad Debt ,_ 2 2 2 3 2 Charity 2 2 2 1 2 TABLE lV-C 2017 Charges per Discharge/Visit ($) HCH St. Teresa Acute 40,000 38,200 SNF 30,000 28,000 Rehab 40,000 38,000 Home Health 400 300 Emergency 1,600 1,500 Outpatient 600 500 SNF = skilled nursing facility 405 Case Study: Hays County Integrated Deiivery System TABLE V Radiology Department Procedures Tech Suppiy Machine Procedure Minutes Expense Minutes Radiology Chest 2-view Chest 4-view Hand Arm Foot Leg Fluoroscopy Ultrasound Abdomen Other Nuclear Medicine Scan CT Head without contrast Head with contrast Body without contrast Body with contrast Case Study: Hays County Integrated Delivery System TABLE Vl-A Salary Survey of Area Hospitals Average Hourly Rates (in dollars, without benefits). December 2017 Position HCH St. Teresa Chief Executive Ofcer 595.00 595.00 Chief Operating Ofcer 390.00 386.00 Chief Nursing Ofcer 175.00 172.00 Director Clinical Services 230.00 226.00 Director Support Services 150.00 149.00 Chief Medical Ofcer 295.00 291.00 Chief Financial Ofcer 312.00 280.00 Chief Compliance Ofcer 140.00 135.00 Chieflnformation Ofcer 225.00 222.00 Head Nurse 43.00 38.00 Staff RN 37.40 33.00 Staff LPN 24.70 21.00 Nursing Assistant 14.80 11.00 Laboratory Tech 31.68 28.00 Radiology Tech 29.72 26.00 Food Sewer 12.45 9.45 Housekeeper 12.41 9.00 Administrators Below Chiefs 40.73 37.00 Clerk 20.23 17.00 Respiratory Therapist 30.14 27.25 Case Study: Hays County integrated Delivery System MEETING WITH DR. SPOK Dr. Spok, hospital medical director, tells you: Most doctors have been on the medical staff for at leastten years. There is little lo] to the hospital, and most doctors also have admitting privileges at St. Teresa's, a ne hospital with better facilities. While it is a hassle for the doctors to drive the 25 m from San Marcos to St. Teresa's to see patients, there are a few good reasons for doctors to admit their patients to St. Teresa's. St. Teresa's has a hospitalist and 53 physicians for menial service assign ments like committee work (a practice that Colin has refused to implement). ' ' MEETING WITH MR. SALTER Mr. Salter, chief executive ofcer, states: [just don't understand why we are losing money. I spent a considerable amount oftime 5, l recruiting new doctors while keeping the existing doctors happy. The new, younger ,: doctors just don't seem to have a sense ofloyalty to County. Furthermore, I've tried to , { establish a \"family atmosphere" for our employees that stresses getting along well with 7 others in return forjob security. Everyone seems happyeveryone except Mr. Finance Myway, whom you'll be replacing. He and I both started in January 2015 and he seemed increasingly frustrated with the way 1 do things herehe just didn't t in. I tried to. accommodate him by implementing some of his recommendations, even though they were against my better judgmentlike charging visitors for parking, which generated $100,000 in other operating revenue in 2017, but I have discontinued the practice for 2018 because no other organization in San Marcos, other than the university, charges for parking. And when 1 announced that l was bringing in more business to the hos- pital by entering into a two-year capitated managed care agreement with the city (it expires this month) -we get $250 per month per family for taking care of the 300 city employees and their families, whether they're sick or notMr. Myway threw a t at an executive team meeting. He claimed that my decisions were driving County deeper into the red, and as a result, I had to show Mr. Myway the highway for insubordination. That happened last month. Mr. Salter has asked you to do the following [Nora Steps in the case correspond to chapters in the textbook]: 1. I would like you to make a fteenminute, 25slide PowerPoint presentation during our board strategic planning retreat regarding the effects of the economy [see appendix 1.2 in chapter 1] on the healthcare industry. Case Study: Hays County Integrated Delivery System expense budget using the stafng found in Table VI-B, in statement of operations format including detailed footnotes explaining any changes in the numbers. I would like to see at least four di'erent expense scenarios: (1) Maintain expenses at 2017 levels after adjusting for volumes and mandated expenditures identied in earlier steps (2) Maintain expenses at 2017 levels after adjusting for volumes and mandated expenditures identied in earlier steps and bartering all requests (i.e., raises, additional personnel, etc.) (3) Cut expenses (from expense scenario 1) to break even in 2018 (4) Cut expenses (Front expense scenario 1)_ to break even in 2.018 and recover rm! year 20171052: 15. Calculate the nancial impact of buying a CT [computed tomography] unit that would cost $3 million, would have a ve-year useil life, would have a 10 percent salvage value, would have a prot per procedure of $400, and would generate an estimated volume of450 procedures per year. The bank tells me the discount rate should be 10 percent. If the project loses money, let me know how many procedures in addition to the 450 projected per year we would need to generate to break even. Our longterm debt represents the remaining balance on a 30year loan taken out in 1997 at 7 percent with options to renance every ten years. If we renance for the remaining ten years at 3 percent, how much interest expense will we save over the remainder qfthe loan? 16. Please give me your thoughts on the operational and nancial implications of the ACA of2010 and MACRA [Medicare Access and CHIP Reauthorization Act] of 2015 on our hospital. MEETING WITH MR. WANNABE Mr. Wannabe, the chief operating ofcer and a recent graduate from a program in healthcare administration, expresses the following concerns regarding the hospital: I It's easy to understand how we lost money lastyearMr. Salterjust won't say no to the doctors, or the nurses, for that matter. Our revenue is down for a variety of reasons and 399 little loyalty a's, a newer he 25 miles ;on5 for the st and pays that County ount oftime aw, younger . I've tried to mg well with Mr. Finance 1 he seemed in. I tried to though they h generated practice for iity, charges . to the has n the city (it the 300 city 1W 3 t at an deeper into nation.That correspond to aresentation 3f the :tt'y. And I would like you to make a fteen-minute, 2.5slide PowerPoint presentation to the medical staff regarding the role of the CFO and the roles of the primary direct reports to you. Develop a statement of operations for 2017 using Tables ii, IVA, IVB, and IVC [at the end of this case study} and a balance sheet for 2017 (you can assume the format and numbers are correct on the 2016 balance sheet in Table I, and you can further assume that all balances on the 2016 balance sheet carry forward to the 2017 balance sheet with the exception of accounting for the prot or loss from the 2017 statement of operations). Analyze the nancial statements using ratio analysis with benchmarks found in Table III and identify strengths and weal-messes and then make recommendations for improvement in 2018. The Treasury Department has issued nal regulations on the ACA [AHordable Care Act] requirements for not-forprot hospitals. Hospitals must be in compliance with regulations beginning in 2016. Please explain the requirements to me; please identify the penalties for noncompliance found in the IRS regulations (501(1)); and please recommend ways to protect our tax- exempt status. Please explain the concept of cost shifting to me and tell me why it has become increasingly less effective in generating more income. \\What is taking its place in generating more income? Medicare talks a lot about value-based purchasing. What is it and why is Medicare talking about it? Are there implications to our hospital? Explain the Medicaid expansion and why some states expanded Medicaid and why some states did not expand Medicaid. What are the nancial implications of Medicaid expansion to our hospital (be specic with revenue forecasts)? Analyze my capitated managed care agreement with the city. Using differential cost analysis for 2017 data, tell me the hill cost prot/loss and the differential cost prot/loss. Should we renew the contract for next year at present rates, or should we ask for a rate increase and if so, how much rate increase do we need to cover our fuli cost? To cover our diEerential cost? Our imaging department is in violation ofantiiIust statutes because it produced charges using relative value units developed by another organization. You must establish new relative value units and then set 2017 imaging rates using activitybased costing. Total imaging expenses for 2017 are projected to be $6.5 million, and the imaging manager has already nished some of the work that you will need (see Table V). Case Study: Hays County Integrated Delivery System . 'W'hat is the best ratio for measuring accounts receivable performance? i is our hospital doing? What are your recommendations on improving- , accounts receivable performance? . I also need your assistance in calculating the following economic order I quantity [Qe] given new data for 2.017. Our inventory generally follows-{31' Paretos Law; therefore, I have emphasized controlling those items representing the majority of our inventory activity. One of those items '_ [intravenous] setups. Our current situation is as Follows: ' 2016 Price $50 for each IV setup 2017 Demand 50,000 2017 Ordering cost $25 2017 Interest 6.25% 2017 Holding cost $0.50 The W distributor would like to distribute a new model setup in .1' at the same price, but he tells us that he 15 willing to reduce our Carrying I- ' making monthly deliveries. After discussing this proposal with Ms. Care, I "j_ ered that training will be required for the new setup. Ms. Cate believes, and ] distributor agrees, that each registered nurse will be required to attenda ' - ll seminar. I'm not sure where we put this training cost in the total cost f0 1- : ' 1, Ms. Care tells me there are signicant quality advantages with the newscttp' she would prefer the new setup. What do you think? If we lose money on v?" model, what price can we negotiate with the IV distributor to cover curious? . I would like you to develop a veyear strategic nancial plan for Hays County IDS inciuding benchmarked nancial metrics. Our strategic pk .. calls for a replacement facility in about ten years. 7 . For 2018. develop a statistical budget using regression analysis; then . ' ' -. a revenue budget (using a nancial model, determine whether to incrmsc .'.' charges found in Table W-C and ifso, how much) and then develop an l.' 9 8 Case Study Hays County Integrated Dellvery System 10. Dr. Garcia is thinking about retiring this year and has asked us if we - buy her practice. She would like annual income of $250,000 for the u - " years. If we can put the purchase price in an annuity that earns 4 pe -- \" year compounded annually, what is the purchase price necessary to - - 3 her desired income? What other factors should we consider before b ' ' physician practice? What is your recommendation