Answered step by step
Verified Expert Solution
Question
1 Approved Answer
After the insurance carrier makes a decision on a claim and the practice receives and posts the payment, the patient's balance must be calculated. The
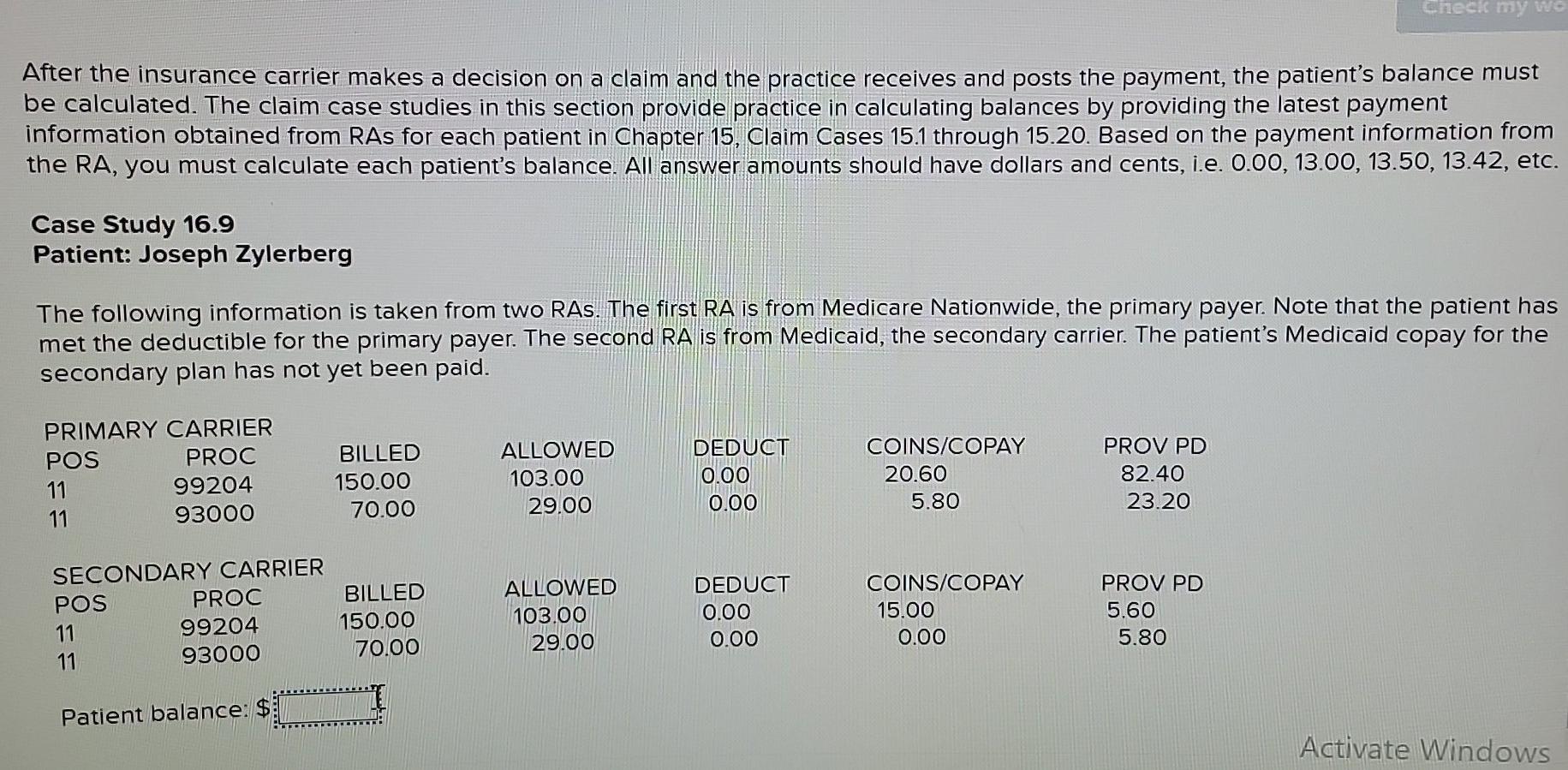
After the insurance carrier makes a decision on a claim and the practice receives and posts the payment, the patient's balance must be calculated. The claim case studies in this section provide practice in calculating balances by providing the latest payment information obtained from RAs for each patient in Chapter 15 , Claim Cases 15.1 through 15.20. Based on the payment information from the RA, you must calculate each patient's balance. All answer amounts should have dollars and cents, i.e. 0.00,13.00,13.50,13.42, etc. Case Study 16.9 Patient: Joseph Zylerberg The following information is taken from two RAs. The first RA is from Medicare Nationwide, the primary payer. Note that the patient has met the deductible for the primary payer. The second RA is from Medicaid, the secondary carrier. The patient's Medicaid copay for the secondary plan has not yet been paid. Patient balance: $ Activate Windows
Step by Step Solution
There are 3 Steps involved in it
Step: 1

Get Instant Access to Expert-Tailored Solutions
See step-by-step solutions with expert insights and AI powered tools for academic success
Step: 2

Step: 3

Ace Your Homework with AI
Get the answers you need in no time with our AI-driven, step-by-step assistance
Get Started