Answered step by step
Verified Expert Solution
Question
1 Approved Answer
Florida Blue: the blues of the Affordable Care Act A graduate of Colgate, Pat Geraghty spent 18 years with Prudential, before moving on to
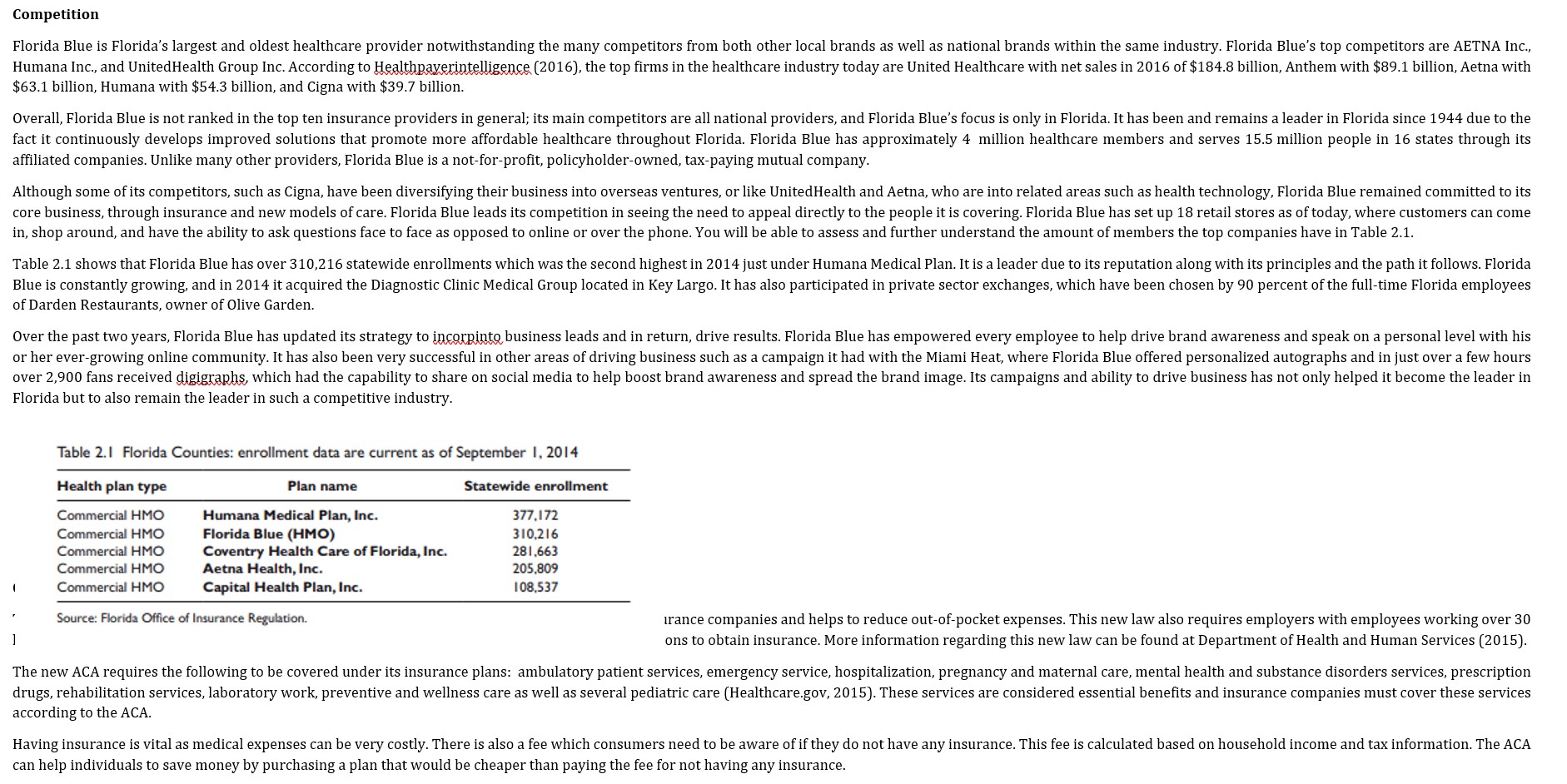
Florida Blue: the blues of the Affordable Care Act A graduate of Colgate, Pat Geraghty spent 18 years with Prudential, before moving on to spend an additional 9 years with the Blue affiliate in New Jersey before being hired in 2008 as Chief Executive Officer (CEO) at the Minnesota Blue. When former Florida Blue leader Robert Lufrano decided to retire in 2011, he advised Geraghty of the position. This was an opportunity Geraghty said he could not pass on; he was excited by the challenges the Florida location would bring, the "size, scope, complexity of the assignment" according to Mark Vogel (2014). However, as Geraghty took the reins of Florida Blue, the health insurance industry was faced with an important issue that would change the landscape of the company. In 2010, the government passed the Patient Protection and Affordable Care Act (ACA) law, otherwise known as Obamacare. This piece of legislation, which was championed by the president himself, mandates that all citizens be eligible for health insurance. The implementation of the ACA posed a threat to Florida Blue's overall performance in the market, as now there would be an increase in competition, and the lower insurance prices would mean that revenue streams would slow down. That being said, it was up to Geraghty to come up with a solution that would satisfy all parties involved and ensure that the company kept its position as a market leader. Company information Florida Blue is a subsidiary of Blue Cross Blue Shield Association, which is a federation of 36 separate health insurance providers in the United States. Florida Blue is one of the providers that cover the whole state of Florida. As currently constituted, Florida Blue is the oldest and largest healthcare provider in the state, with approximately 4.3 million members and 11,500 employees within the state. Florida Blue was founded in 1944 in Jacksonville, Florida, with a staff of only four individuals. The company was originally called the Florida Hospital Service Corporation (FHSC), but its name was changed to Blue Cross of Florida. Its competition, Florida Medical Services Association, was formed in 1946 with similar goals as FHSC. Eventually, these two companies merged in 1980 to create Blue Cross and Blue Shield of Florida, a name that was kept until 2012, when the company underwent a rebranding campaign and changed its name to Florida Blue in order to make it easier for its customers to remember it. Florida Blue's organizational structure is divided into three distinct businesses: Health Business, Government Business, and Life and Specialty Ventures. The Health business is the core business, it is the one in charge of the individual insurance policies. With its 4.2 million members, it currently owns approximately 29 percent of the market, more than double that of its nearest competitor. Government business concerns Medicare and the Affordable Care Act, and is administered by a subsidiary called First Coast Service Options. The Life and Specialty Ventures business specializes in selling policies to businesses and other groups, which include dental, health, and life insurance. Florida Blue's mission statement reads "To help people and communities achieve better health," and its vision states "A company focused primarily on the health industry, delivering value through an array of meaningful choices." These two statements exemplify the core values of respect, integrity, imagination, courage, and excellence. These are values that the company tries to uphold through its services and customer support. Industry information In 2014, the insurance industry recorded revenue totaling $1.1 billion. Of this figure, 56 percent was for life and health insurance, while 44 percent accounted for property and casualty. According to a 2015 report by IBIS World Report, the Health and Medical Insurance industry, which is made up of carriers of private, group and public health, medical, dental insurance, was characterized by slow growth 5 years ago as a result of reduced employer coverage and continued consumer deleveraging. However, consistent increases in healthcare expenditure and medical cost inflation, as well as a sharp decline in the uninsured rate, have driven industry growth in recent years. Growth is expected to continue in the ensuing years, the assumption is, as the baby boomers aged, their need for more medical coverage will increase. Their retirement will also help to boost Medicare expenditure. (Ibis World Report, 2017) To be successful in the health insurance industry, many partnerships and alliances had to be forged. As such, the health insurance market is connected with many sectors of the healthcare system, along with many other private partners. Health insurers act as a third party between the patients and healthcare. The health insurers reimburse the healthcare provider on behalf of the patient for services rendered. The health insurer also provides guidelines on the amount of coverage a patient has available to him/her. Most health insurance plans are managed care plans (Health Maintenance Organizations [HMOS], Preferred Provider Organizations [PPOS]) rather than indemnity or traditional health insurance plans that provide unlimited reimbursement for a fixed premium, according to Austin and Hungerford, 2009. The Health and Medical Insurance Industry is in the mature stage of its economic life cycle; this stage is characterized by a slowdown in technological development and wholehearted market acceptance of the industry's products and services. Industry value added (IVA), which measures an industry's contribution to the overall economy, is expected to increase at an annualized rate of 2.7% during the 10 years to 2020. In contrast, US GDP is projected to grow at an annualized rate of 2.2% during the same period. These figures signify that the industry's share of the US economy is holding steady, as the industry is growing at close to the same rate as the rest of the economy. (IBIS World Report, 2017) According to Cox, Ma, Claxton, and Levitt (2014), The individual health insurance market historically has been highly concentrated, with only modest competition in most states. At the time the Affordable Care Act was signed into law in 2010, a single insurer had at least half of the individual market in 30 states and the District of Columbia. While a dominant insurer may be able to negotiate lower rates from hospitals and physicians, without significant competitors or regulatory oversight, there is no guarantee that those savings would be passed along to consumers. The industry products include Pharmacy Benefit Management (PBM), Preferred Provider Organization (PPO), High-deductible Health Plans (HDHPS), Health Maintenance Organization (HMO), Point-of-service (POS), Fee-for-service (FFS), Medicaid (via private firms), and Medicare (via private firms). Competition Florida Blue is Florida's largest and oldest healthcare provider notwithstanding the many competitors from both other local brands as well as national brands within the same industry. Florida Blue's top competitors are AETNA Inc., Humana Inc., and UnitedHealth Group Inc. According to Healthpaverintelligence (2016), the top firms in the healthcare industry today are United Healthcare with net sales in 2016 of $184.8 billion, Anthem with $89.1 billion, Aetna with $63.1 billion, Humana with $54.3 billion, and Cigna with $39.7 billion. Overall, Florida Blue is not ranked in the top ten insurance providers in general; its main competitors are all national providers, and Florida Blue's focus is only in Florida. It has been and remains a leader in Florida since 1944 due to the fact it continuously develops improved solutions that promote more affordable healthcare throughout Florida. Florida Blue has approximately 4 million healthcare members and serves 15.5 million people in 16 states through its affiliated companies. Unlike many other providers, Florida Blue is a not-for-profit, policyholder-owned, tax-paying mutual company. Although some of its competitors, such as Cigna, have been diversifying their business into overseas ventures, or like UnitedHealth and Aetna, who are into related areas such as health technology, Florida Blue remained committed to its core business, through insurance and new models of care. Florida Blue leads its competition in seeing the need to appeal directly to the people it is covering. Florida Blue has set up 18 retail stores as of today, where customers can come in, shop around, and have the ability to ask questions face to face as opposed to online or over the phone. You will be able to assess and further understand the amount of members the top companies have in Table 2.1. Table 2.1 shows that Florida Blue has over 310,216 statewide enrollments which was the second highest in 2014 just under Humana Medical Plan. It is a leader due to its reputation along with its principles and the path it follows. Florida Blue is constantly growing, and in 2014 it acquired the Diagnostic Clinic Medical Group located in Key Largo. It has also participated in private sector exchanges, which have been chosen by 90 percent of the full-time Florida employees of Darden Restaurants, owner of Olive Garden. Over the past two years, Florida Blue has updated its strategy to incorpinto business leads and in return, drive results. Florida Blue has empowered every employee to help drive brand awareness and speak on a personal level with his or her ever-growing online community. It has also been very successful in other areas of driving business such as a campaign it had with the Miami Heat, where Florida Blue offered personalized autographs and in just over a few hours over 2,900 fans received digigraphs, which had the capability to share on social media to help boost brand awareness and spread the brand image. Its campaigns and ability to drive business has not only helped it become the leader in Florida but to also remain the leader in such a competitive industry. Table 2.1 Florida Counties: enrollment data are current as of September 1, 2014 Health plan type Plan name Statewide enrollment Commercial HMO Commercial HMO Commercial HMO Commercial HMO Commercial HMO Humana Medical Plan, Inc. Florida Blue (HMO) 377,172 310,216 Coventry Health Care of Florida, Inc. 281,663 Aetna Health, Inc. Capital Health Plan, Inc. 205,809 108,537 Source: Florida Office of Insurance Regulation. irance companies and helps to reduce out-of-pocket expenses. This new law also requires employers with employees working over 30 ons to obtain insurance. More information regarding this new law can be found at Department of Health and Human Services (2015). The new ACA requires the following to be covered under its insurance plans: ambulatory patient services, emergency service, hospitalization, pregnancy and maternal care, mental health and substance disorders services, prescription drugs, rehabilitation services, laboratory work, preventive and wellness care as well as several pediatric care (Healthcare.gov, 2015). These services are considered essential benefits and insurance companies must cover these services according to the ACA. Having insurance is vital as medical expenses can be very costly. There is also a fee which consumers need to be aware of if they do not have any insurance. This fee is calculated based on household income and tax information. The ACA can help individuals to save money by purchasing a plan that would be cheaper than paying the fee for not having any insurance. Enrollment period is also an important part of purchasing an insurance plan. The enrollment period to purchase via the marketplace is November 1, 2017December 15, 2017. This is to purchase plans as well as renew plans for the new 2018 year. Under circumstances there may be times where an individual may be eligible based upon on a life event to obtain insurance while not in the current enrollment period. Insurance can be purchased via the marketplace on the healthcare.gov website. An application must be completed to begin the process; from there many different insurance plans will be shown with coverage options. The individual then can select the plan that is right for them. Florida Blue, a Florida based insurance plan, offers many plans under the ACA. There are four plans to choose from: Bronze, Silver, Gold, and Platinum. Bronze covers 60 percent, Silver covers 70 percent, Gold covers 80 percent, and Platinum covers 90 percent of medical expenses (Blue Cross and Blue Shield Florida, 2015). Each plan is designed to cover the essential benefits, which is required by the ACA. However, monthly fees and out-of-pocket expenses vary depending on the plan and income level of the individual. In order to choose the plan that suits the individual the best it should be noted that the Bronze plan has the lowest monthly premiums making it the most affordable option; however, it does have significantly higher deductibles as well as the most out-of-pocket expenses. The Platinum plan has the highest monthly premium but has low deductibles as well as fewer out-of-pocket fees. These are important factors when deciding on an insurance policy. Florida Blue also offers an option called catastrophic health insurance plans, which have very low monthly premiums but have a very high deductible of $6,850. This may be a viable option for a healthy individual just needing coverage in case of an emergency and can be used to avoid the fee for not obtaining an insurance plan. Florida Blue plans can be purchased several ways. One way is through the general marketplace on the healthcare.gov website where multiple insurance carriers can be viewed. Insurance can also be purchased direct through a Florida Blue agent or in one of the 18 retail centers. Insurance plans also must be purchased during the open enrollment period, which is November 1, 2017-December 15, 2017. The Florida Blue bronze plan for a typical healthy 25-year-old costs $194 a month. This plan also has a deductible of $6,850 and an out-of-pocket maximum of $6,850. Once the deductible for this plan is met, there is no charge for emergency room care, generic prescriptions, doctors and specialists visits (Department of Health and Human Services, 2015). A Silver plan from Florida Blue has a monthly premium of $219, a deductible of $6,100 and an out-of-pocket expense maximum of $6,850. This plan has several co-payments, for an emergency room visit co-payment is $600 after the deductible is met. Generic prescription drugs costs $30 after the deductible is met and primary doctor visits cost $65 and specialists $95 after the deductible is met (Department of Health and Human Services, 2015). Florida Blue's Gold plan has a monthly premium of $290 and a deductible of $1,600 with a maximum out-of-pocket expense of $3,500. This plan has several co-payments, for an emergency room visit, generic drug coverage, and doctors including specialists' visits it is 10 percent of coinsurance after the deductible is met (Department of Health and Human Services, 2015). For a Platinum insurance plan it has a monthly premium of $574, a deductible of $800, and an out-of-pocket maximum of $2,500. There are several co-payments under this plan. for an emergency room visit it is 10 percent of coinsurance once the deductible is met, generic drugs are $10, primary doctors are $15, and specialists are $20 (Department of Health and Human Services, 2015). This is a sampling of the plans and deductibles Florida Blue offers and varies based upon age, income, and other factors. This information was obtained through the health insurance marketplace under the information of a generally healthy 25-year-old nonsmoking female. Consumers who want to learn more can visit Floridablue.com as well as healthcare.gov. The issues The Affordable Care Act is a law that requires individuals to be covered by health insurance. The law places stricter guidelines on insurance companies and helps to reduce consumers' out-of-pocket expenses. As a result, insurance providers are coming up with new ways to earn a profit. The guidelines enforced directly affect the bottom line of insurance companies and in order to remain successful, plans need to do more than simply sell health insurance. What did they do? In August 2013 Florida insurance regulators ruled to allow Florida Blue to restructure into a not-for-profit mutual holding organization (Kennedy, 2013). Florida Blue became public in this transition, but due to several conflicts of interest was not allowed to sell stock to outside investors. The company can, however, transfer assets to its mutual holding company. In September 2014 Guide Well launched as the parent brand over a family of brands, including Florida Blue. According to Chairman and CEO, Pat Geraghty, GuideWell has (Shedden, 2014) "a family of forward-thinking companies focused on helping people and communities achieve better health." In January 2015 Florida Blue reportedly laid off 150 employees throughout the state. According to Paul Kluding, Senior Director of Public Relations at Florida Blue, "The healthcare industry is undergoing unprecedented change. In order for organizations to adapt, they must tightly manage costs and look for effective solutions that continue to provide customers with the most affordable healthcare choices possible" (Elmore, 2015). This change in the healthcare industry is the Affordable Care Act. As part of the development of the parent brand, GuideWell went through a reorganization to put leadership in place. According to GuideWell news (PR Newswire, 2014), Ren Lerer, M.D. [was] appointed President of Florida Blue and the GuideWell group of companies which includes GuideWell Health, GuideWell Connect and Diversified Service Options, Inc. Lerer will report to Chairman and Chief Executive Officer Patrick J. Geraghty as part of the newly created Office of the CEO. Prakash Patel was named Chief Operating Officer (COO) of GuideWell effective January 2015. The ACA law rules for all citizens to be eligible for health insurance. This transformation in healthcare has allowed low-income families to qualify for subsidies and earn assistance on healthcare plans. These are "highly subsidized" customers. Florida Blue has altered its marketing strategies to target these highly subsidized customers. The company is focusing on grassroots marketing initiatives that target the highly subsidized customer and the Hispanic community. As a result, marketing efforts have shifted from upper-class families to the lower class and highly subsidized, with a strong push towards Hispanics specifically in Miami, Florida. Guide Well has partnered with a Colombian-based health clinic, Sanitas, to open three initial clinics in Miami, with plans to expand throughout the U.S. inother Hispanic markets. The locations are in Doral, Kendall, and Miami Lakes. While primarily targeting customers seeking care through the ACA individual market, the clinics accept Florida Blue members or cash payments. According to GuideWell (2015), The medical center's entire patient experience will be designed to meet the needs and preferences of those in the local markets, including cultural and linguistic aspects that are critical to resonating with a wide variety of Hispanic groups. Furthermore, there will be additional considerations for patient-engagement programs to address country of origin and assimilation differences amongst the targeted Hispanic cultures. A second clinic platform the brand has developed is Guide Well Emergency Doctors, based in Orlando, Florida. There are currently two locations in Orlando and the business model reflects ER care at urgent care prices. The clinics accept insurance plans from most providers. Pat Geraghty had to decide what action Florida Blue would take in response to an important issue that would change the landscape of the organization. The ACA posed a threat to Florida Blue's overall performance in the market, and Geraghty's solution to this threat was an organizational restructuring placing Guide Well as the mutual holding company over the family of brands, which included Florida Blue. The restructuring has allowed Florida Blue to maintain its positioning as the market leader and expand its products and services outside of the original scope of the health insurance provider Need to follow the below format in solving case analysis: I. Problem II. Objectives III. Areas of Consideration IV. Alternative Course of Action V. Recommendation VI. Plan of Action VII. Potential Problems VIII. Contingent Plan of Action Observe the following format in making your article review: Font style Arial Font size : 12 Spacing : Margin Paper size Number of pages Double 1 inch (top, bottom, left and right) 812 x 11 approximately 6 to 8 pages
Step by Step Solution
There are 3 Steps involved in it
Step: 1

Get Instant Access to Expert-Tailored Solutions
See step-by-step solutions with expert insights and AI powered tools for academic success
Step: 2

Step: 3

Ace Your Homework with AI
Get the answers you need in no time with our AI-driven, step-by-step assistance
Get Started