Answered step by step
Verified Expert Solution
Question
1 Approved Answer
Name of person Start Date BSP Type Terry Jenkins 12/10/2018 Normal/emergency CRU James Street Service setting End date 12/10/2019 Billy Bloggs About the person
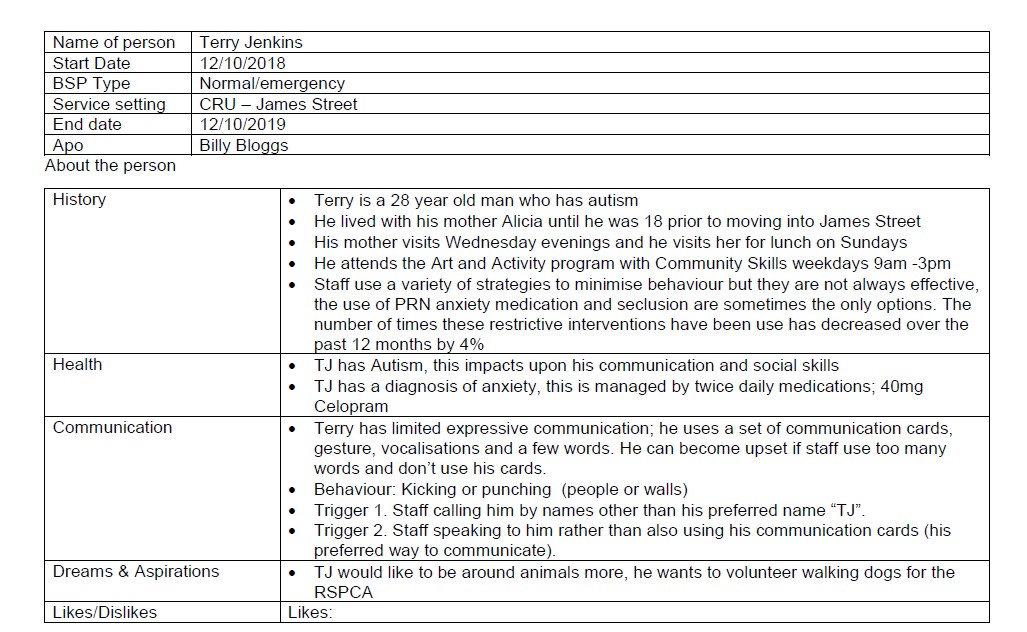
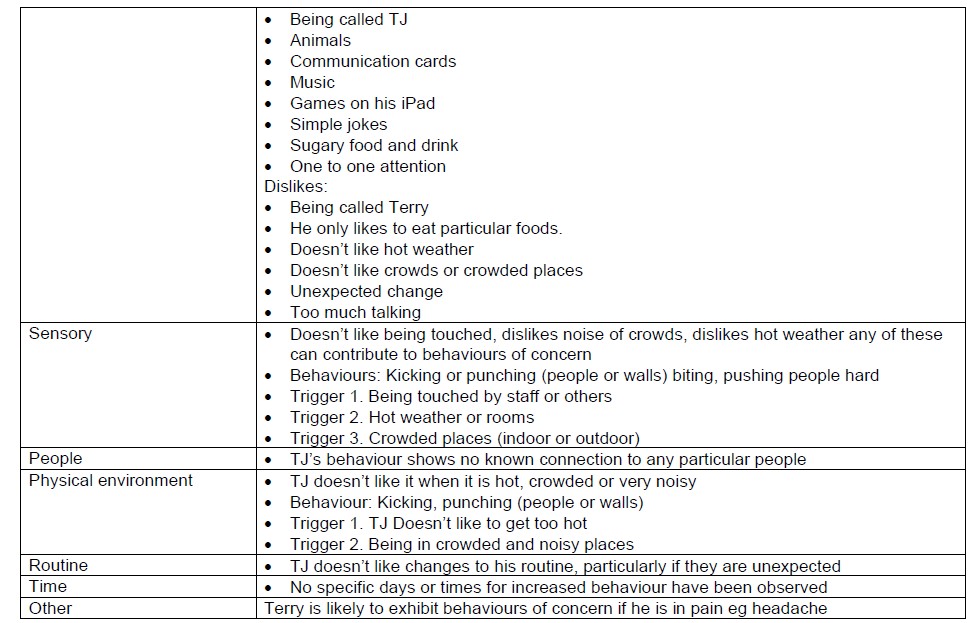
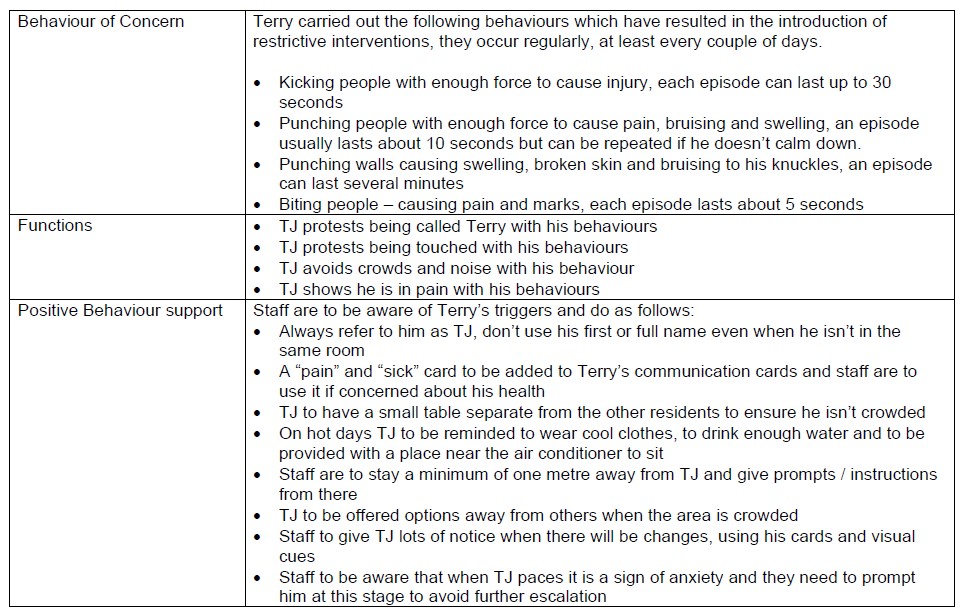


Name of person Start Date BSP Type Terry Jenkins 12/10/2018 Normal/emergency CRU James Street Service setting End date 12/10/2019 Billy Bloggs About the person History Health Communication Dreams & Aspirations Terry is a 28 year old man who has autism He lived with his mother Alicia until he was 18 prior to moving into James Street His mother visits Wednesday evenings and he visits her for lunch on Sundays He attends the Art and Activity program with Community Skills weekdays 9am-3pm Staff use a variety of strategies to minimise behaviour but they are not always effective, the use of PRN anxiety medication and seclusion are sometimes the only options. The number of times these restrictive interventions have been use has decreased over the past 12 months by 4% TJ has Autism, this impacts upon his communication and social skills TJ has a diagnosis of anxiety, this is managed by twice daily medications; 40mg Celopram Terry has limited expressive communication; he uses a set of communication cards, gesture, vocalisations and a few words. He can become upset if staff use too many words and don't use his cards. Behaviour: Kicking or punching (people or walls) Trigger 1. Staff calling him by names other than his preferred name "TJ". Trigger 2. Staff speaking to him rather than also using his communication cards (his preferred way to communicate). TJ would like to be around animals more, he wants to volunteer walking dogs for the RSPCA Likes/Dislikes Likes: Being called TJ Animals Communication cards Music Games on his iPad Simple jokes Sugary food and drink One to one attention Dislikes: Being called Terry He only likes to eat particular foods. Doesn't like hot weather Doesn't like crowds or crowded places Unexpected change Too much talking Doesn't like being touched, dislikes noise of crowds, dislikes hot weather any of these can contribute to behaviours of concern Behaviours: Kicking or punching (people or walls) biting, pushing people hard Trigger 1. Being touched by staff or others Trigger 2. Hot weather or rooms Trigger 3. Crowded places (indoor or outdoor) Sensory People Physical environment TJ's behaviour shows no known connection to any particular people TJ doesn't like it when it is hot, crowded or very noisy Trigger 1. TJ Doesn't like to get too hot Routine Time Other Behaviour: Kicking, punching (people or walls) Trigger 2. Being in crowded and noisy places TJ doesn't like changes to his routine, particularly if they are unexpected No specific days or times for increased behaviour have been observed Terry is likely to exhibit behaviours of concern if he is in pain eg headache Behaviour of Concern Terry carried out the following behaviours which have resulted in the introduction of restrictive interventions, they occur regularly, at least every couple of days. . Kicking people with enough force to cause injury, each episode can last up to 30 seconds Punching people with enough force to cause pain, bruising and swelling, an episode usually lasts about 10 seconds but can be repeated if he doesn't calm down. Punching walls causing swelling, broken skin and bruising to his knuckles, an episode can last several minutes Biting people - causing pain and marks, each episode lasts about 5 seconds Functions TJ protests being called Terry with his behaviours Positive Behaviour support TJ protests being touched with his behaviours TJ avoids crowds and noise with his behaviour . TJ shows he is in pain with his behaviours Staff are to be aware of Terry's triggers and do as follows: Always refer to him as TJ, don't use his first or full name even when he isn't in the same room A "pain" and "sick" card to be added to Terry's communication cards and staff are to use it if concerned about his health TJ to have a small table separate from the other residents to ensure he isn't crowded On hot days TJ to be reminded to wear cool clothes, to drink enough water and to be provided with a place near the air conditioner to sit Staff are to stay a minimum of one metre away from TJ and give prompts / instructions from there TJ to be offered options away from others when the area is crowded Staff to give TJ lots of notice when there will be changes, using his cards and visual cues Staff to be aware that when TJ paces it is a sign of anxiety and they need to prompt him at this stage to avoid further escalation Replacement behaviour and skill teaching Physical and mental wellbeing Goals and objectives De-escalation Restrictive Interventions TJ to be taught by staff to show his name card to remind people he likes to be called TJ TJ to be taught by staff to show his "pain" or "sick" card to staff and point to the area when unwell TJ to be encouraged to go for a walk or use his iPad if he is becoming upset TJ to continue to have his anxiety medication Annual dental and doctors appointments to monitor overall wellbeing TJ will reduce the incidences of behaviours of concern to a maximum of 3 times per week TJ will use his communication cards to tell staff what he wants TJ will go for a walk or use his iPad if he is becoming upset Strategies apply to all TJ's behaviours - kicking, punching, pushing and biting Staff to assess if imminent risk to TJ, staff or others Prompt TJ to use his communication cards to tell you what is wrong, maintain your distance If you can determine the reason address it where possible eg in pain, put Panadol in his medicine cup and ask him to take it. If he won't do this prompt TJ to use go for a walk in the yard or use his iPad to calm down If TJ doesn't respond and continues to escalate remove others from area, ask the other staff person to be on hand Prompt TJ again, invite him to leave the area If escalation continues and no immediate risk stay in the area but away from TJ When he calms down administer PRN anxiety medication If TJ or others in danger then using a firm and calm voice say - "Room please" and point towards it or the nomination seclusion area, once he's there lock the door Once calmer administer PRN anxiety medication PRN Chemical - Diazepam 10mg, oral, maximum 3 per day, minimum re-administration period - 4 hrs TJ benefits from this medication as it calms him down and relaxes him so he can then let staff know what he needs PRN Seclusion - In his room or nominated seclusion area, maximum period of seclusion - 30 minutes TJ calms down when left alone, it make him feel secure and once relaxed he can communicate with staff.
Step by Step Solution
There are 3 Steps involved in it
Step: 1

Get Instant Access to Expert-Tailored Solutions
See step-by-step solutions with expert insights and AI powered tools for academic success
Step: 2

Step: 3

Ace Your Homework with AI
Get the answers you need in no time with our AI-driven, step-by-step assistance
Get Started


