Question
The OB chair believes that with better scheduling, various process improvements, incremental equipment, and other modest changes, her group could reduce LOS from 2.7 days
The OB chair believes that with better scheduling, various process improvements, incremental equipment, and other modest changes, her group could reduce LOS from 2.7 days to 2.5 days and maintain 81% mean occupancy without any more congestion than under the status quo. The cost of implementing all of the chairs recommendations is $85,000.
a. How many fewer beds would be needed in this case to enable 3,650 deliveries per year?
b. If the chairs recommendations had come after the L&D beds in question 1 were added, how many more deliveries (beyond 3,650 per year) could ACH provide?
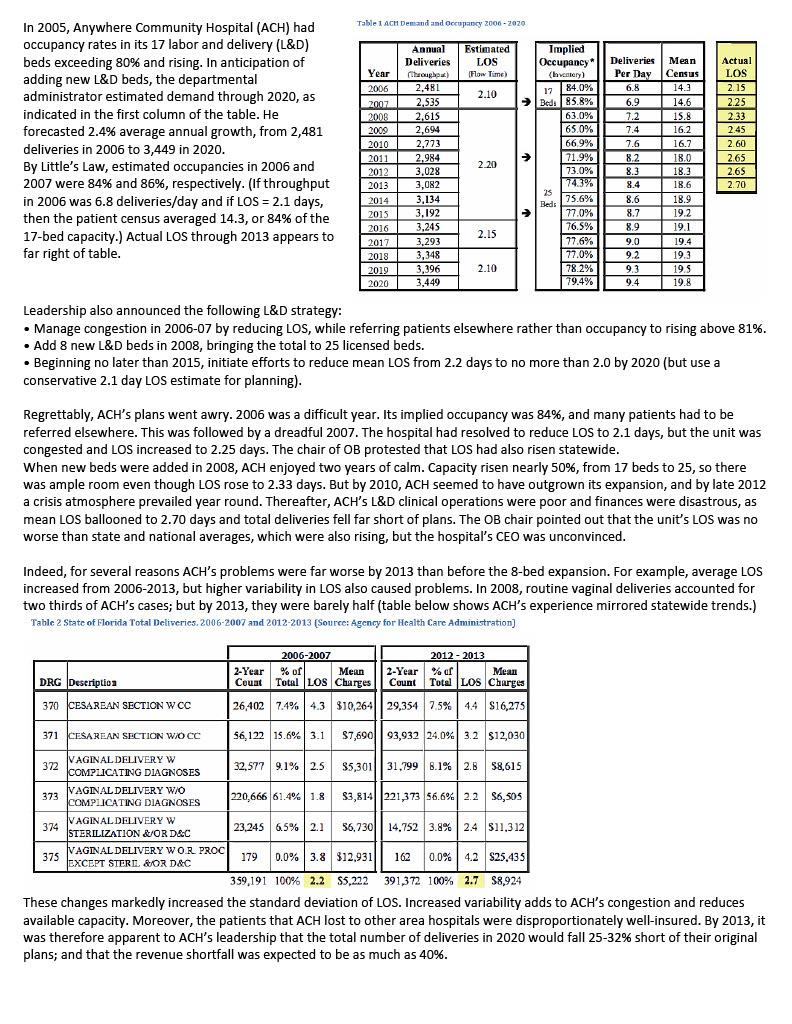
Table 1 ACH Demand and occupancy 2006 - 2020 Deliveries Per Day In 2005, Anywhere Community Hospital (ACH) had occupancy rates in its 17 labor and delivery (L&D) beds exceeding 80% and rising. In anticipation of adding new L&D beds, the departmental administrator estimated demand through 2020, as indicated in the first column of the table. He forecasted 2.4% average annual growth, from 2,481 deliveries in 2006 to 3,449 in 2020. By Little's Law, estimated occupancies in 2006 and 2007 were 84% and 86%, respectively. (If throughput in 2006 was 6.8 deliveries/day and if LOS = 2.1 days, then the patient census averaged 14.3, or 84% of the 17-bed capacity.) Actual LOS through 2013 appears to far right of table. Annunl Deliveries throughod) 2,481 2.535 2,615 2,694 2,773 2,984 3,028 3,082 3,134 3,192 3,245 3,293 3,348 3,396 3,449 Estimated Implied LOS Occupancy* Flow Time) (la vetery) 84.0% 17 2.10 Bedi 85.8% 63.0% 65.0% 66.9% > 71.9% 2.20 73.0% Year 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019 2020 6.8 6.9 7.2 7.4 7.6 8,2 8.3 Mean Census 14.3 14.6 15.8 16.2 16.7 18.0 18.3 18.6 18.9 19.2 19.1 19.4 19.3 19.5 19.8 Actual LOS 2.15 2.25 2.33 2.45 2.60 2.65 2.65 2.70 8.4 2.15 75.6% % Beds 77.0% 76.5% 77.6% 77.0% 78.2% 79.4% 8.6 8.7 8.9 9.0 9.2 9.3 9.4 2.10 Leadership also announced the following L&D strategy: Manage congestion in 2006-07 by reducing Los, while referring patients elsewhere rather than occupancy to rising above 81%. Add 8 new L&D beds in 2008, bringing the total to 25 licensed beds. Beginning no later than 2015, initiate efforts to reduce mean Los from 2.2 days to no more than 2.0 by 2020 (but use a conservative 2.1 day LOS estimate for planning). Regrettably, ACH's plans went awry. 2006 was a difficult year. Its implied occupancy was 84%, and many patients had to be referred elsewhere. This was followed by a dreadful 2007. The hospital had resolved to reduce LOS to 2.1 days, but the unit was congested and LOS increased to 2.25 days. The chair of OB protested that LOS had also risen statewide. When new beds were added in 2008, ACH enjoyed two years of calm. Capacity risen nearly 50%, from 17 beds to 25, so there was ample room even though Los rose to 2.33 days. But by 2010, ACH seemed to have outgrown its expansion, and by late 2012 a crisis atmosphere prevailed year round. Thereafter, ACH's L&D clinical operations were poor and finances were disastrous, as mean LOS ballooned to 2.70 days and total deliveries fell far short of plans. The OB chair pointed out that the unit's LOS was no worse than state and national averages, which were also rising, but the hospital's CEO was unconvinced. Indeed, for several reasons ACH's problems were far worse by 2013 than before the 8-bed expansion. For example, average LOS increased from 2006-2013, but higher variability in LOS also caused problems. In 2008, routine vaginal deliveries accounted for two thirds of ACH's cases; but by 2013, they were barely half (table below shows ACH's experience mirrored statewide trends.) Table 2 State of Florida Total Deliveries. 2006-2007 and 2012-2013 (Source: Agency for Health Care Administration) DRG Description 2006-2007 2012 - 2013 2-Year % of Mean 2-Year % of Mean Couat Total LOS Charges Count Total LOS Charges 26,402 7.4% 4.3 310,264|| 29,354 7.5% 44 816,275 370 CESAREAN SECTION W CC W 371 CESAREAN SECTION WO CC 56,122 15.6% 3.1 $7,69093,932 24.0% 3.2 $12,030 VAGINAL DELIVERY W 372 COMPLICATING DIAGNOSES 32,577 9.1% 2.5 $5,301||% 31.799 8.1% 2.8 58,615 VAGINAL DELIVERY W/O 373 COMPLICATING DIAGNOSES 220,666 61.4% 1.8 $3,814221,373 56.6% 2.2 $6,505 374 VAGINAL DELIVERY W 23.245 6.5% 2.1 STERILIZATION &/OR D&C 56,730|| 14.752 3.8% 2.4 $11.312 VAGINAL DELIVERY WORL PROC 375 179 0.0% 3.8 $12,931 162 JEXCEPT STERIL & OR D&C 0.0% 4.2 $25,435 359,191 100% 2.2 $5,222 391,372 100% 2.7 $8,924 These changes markedly increased the standard deviation of LOS. Increased variability adds to ACH's congestion and reduces available capacity. Moreover, the patients that ACH lost to other area hospitals were disproportionately well-insured. By 2013, it was therefore apparent to ACH's leadership that the total number of deliveries in 2020 would fall 25-32% short of their original plans; and that the revenue shortfall was expected to be as much as 40%. Table 1 ACH Demand and occupancy 2006 - 2020 Deliveries Per Day In 2005, Anywhere Community Hospital (ACH) had occupancy rates in its 17 labor and delivery (L&D) beds exceeding 80% and rising. In anticipation of adding new L&D beds, the departmental administrator estimated demand through 2020, as indicated in the first column of the table. He forecasted 2.4% average annual growth, from 2,481 deliveries in 2006 to 3,449 in 2020. By Little's Law, estimated occupancies in 2006 and 2007 were 84% and 86%, respectively. (If throughput in 2006 was 6.8 deliveries/day and if LOS = 2.1 days, then the patient census averaged 14.3, or 84% of the 17-bed capacity.) Actual LOS through 2013 appears to far right of table. Annunl Deliveries throughod) 2,481 2.535 2,615 2,694 2,773 2,984 3,028 3,082 3,134 3,192 3,245 3,293 3,348 3,396 3,449 Estimated Implied LOS Occupancy* Flow Time) (la vetery) 84.0% 17 2.10 Bedi 85.8% 63.0% 65.0% 66.9% > 71.9% 2.20 73.0% Year 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019 2020 6.8 6.9 7.2 7.4 7.6 8,2 8.3 Mean Census 14.3 14.6 15.8 16.2 16.7 18.0 18.3 18.6 18.9 19.2 19.1 19.4 19.3 19.5 19.8 Actual LOS 2.15 2.25 2.33 2.45 2.60 2.65 2.65 2.70 8.4 2.15 75.6% % Beds 77.0% 76.5% 77.6% 77.0% 78.2% 79.4% 8.6 8.7 8.9 9.0 9.2 9.3 9.4 2.10 Leadership also announced the following L&D strategy: Manage congestion in 2006-07 by reducing Los, while referring patients elsewhere rather than occupancy to rising above 81%. Add 8 new L&D beds in 2008, bringing the total to 25 licensed beds. Beginning no later than 2015, initiate efforts to reduce mean Los from 2.2 days to no more than 2.0 by 2020 (but use a conservative 2.1 day LOS estimate for planning). Regrettably, ACH's plans went awry. 2006 was a difficult year. Its implied occupancy was 84%, and many patients had to be referred elsewhere. This was followed by a dreadful 2007. The hospital had resolved to reduce LOS to 2.1 days, but the unit was congested and LOS increased to 2.25 days. The chair of OB protested that LOS had also risen statewide. When new beds were added in 2008, ACH enjoyed two years of calm. Capacity risen nearly 50%, from 17 beds to 25, so there was ample room even though Los rose to 2.33 days. But by 2010, ACH seemed to have outgrown its expansion, and by late 2012 a crisis atmosphere prevailed year round. Thereafter, ACH's L&D clinical operations were poor and finances were disastrous, as mean LOS ballooned to 2.70 days and total deliveries fell far short of plans. The OB chair pointed out that the unit's LOS was no worse than state and national averages, which were also rising, but the hospital's CEO was unconvinced. Indeed, for several reasons ACH's problems were far worse by 2013 than before the 8-bed expansion. For example, average LOS increased from 2006-2013, but higher variability in LOS also caused problems. In 2008, routine vaginal deliveries accounted for two thirds of ACH's cases; but by 2013, they were barely half (table below shows ACH's experience mirrored statewide trends.) Table 2 State of Florida Total Deliveries. 2006-2007 and 2012-2013 (Source: Agency for Health Care Administration) DRG Description 2006-2007 2012 - 2013 2-Year % of Mean 2-Year % of Mean Couat Total LOS Charges Count Total LOS Charges 26,402 7.4% 4.3 310,264|| 29,354 7.5% 44 816,275 370 CESAREAN SECTION W CC W 371 CESAREAN SECTION WO CC 56,122 15.6% 3.1 $7,69093,932 24.0% 3.2 $12,030 VAGINAL DELIVERY W 372 COMPLICATING DIAGNOSES 32,577 9.1% 2.5 $5,301||% 31.799 8.1% 2.8 58,615 VAGINAL DELIVERY W/O 373 COMPLICATING DIAGNOSES 220,666 61.4% 1.8 $3,814221,373 56.6% 2.2 $6,505 374 VAGINAL DELIVERY W 23.245 6.5% 2.1 STERILIZATION &/OR D&C 56,730|| 14.752 3.8% 2.4 $11.312 VAGINAL DELIVERY WORL PROC 375 179 0.0% 3.8 $12,931 162 JEXCEPT STERIL & OR D&C 0.0% 4.2 $25,435 359,191 100% 2.2 $5,222 391,372 100% 2.7 $8,924 These changes markedly increased the standard deviation of LOS. Increased variability adds to ACH's congestion and reduces available capacity. Moreover, the patients that ACH lost to other area hospitals were disproportionately well-insured. By 2013, it was therefore apparent to ACH's leadership that the total number of deliveries in 2020 would fall 25-32% short of their original plans; and that the revenue shortfall was expected to be as much as 40%Step by Step Solution
There are 3 Steps involved in it
Step: 1

Get Instant Access to Expert-Tailored Solutions
See step-by-step solutions with expert insights and AI powered tools for academic success
Step: 2

Step: 3

Ace Your Homework with AI
Get the answers you need in no time with our AI-driven, step-by-step assistance
Get Started