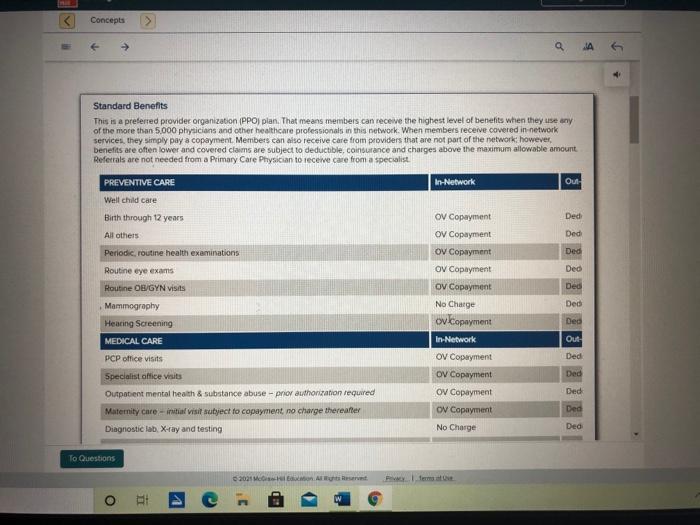
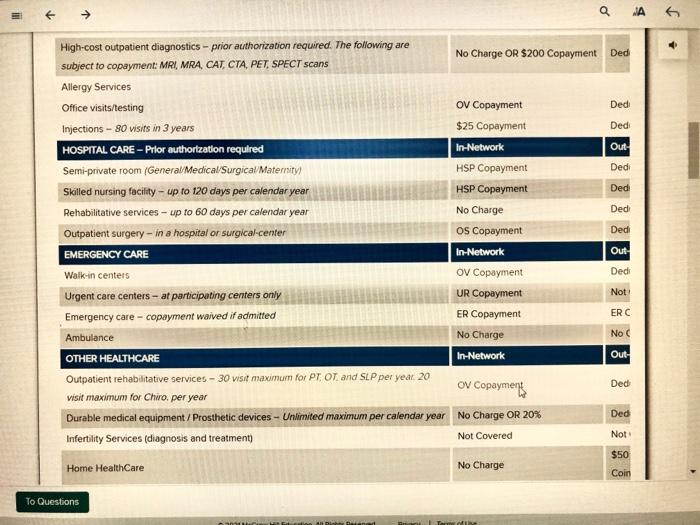
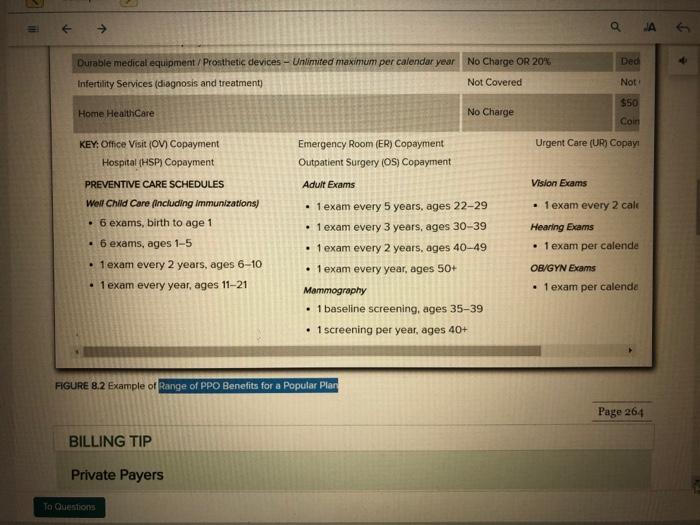
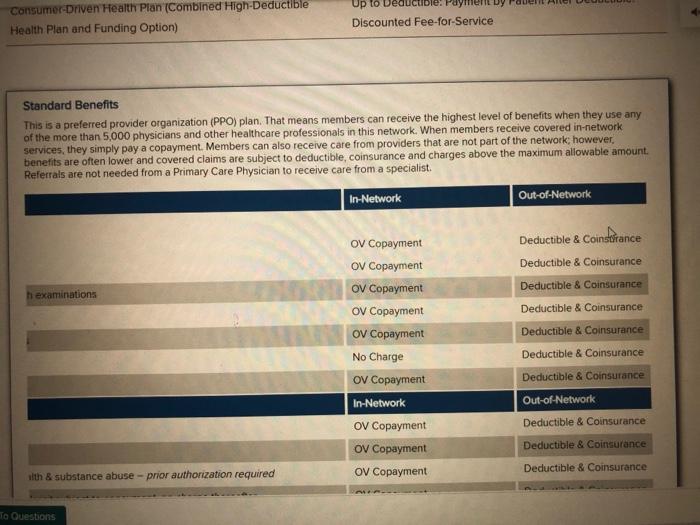
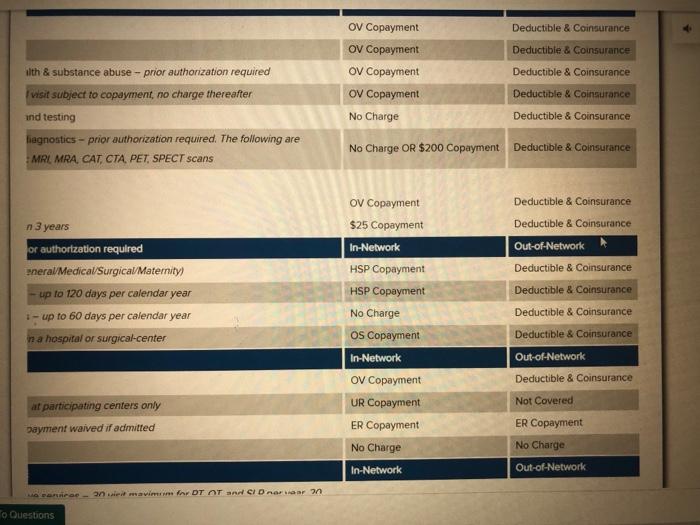
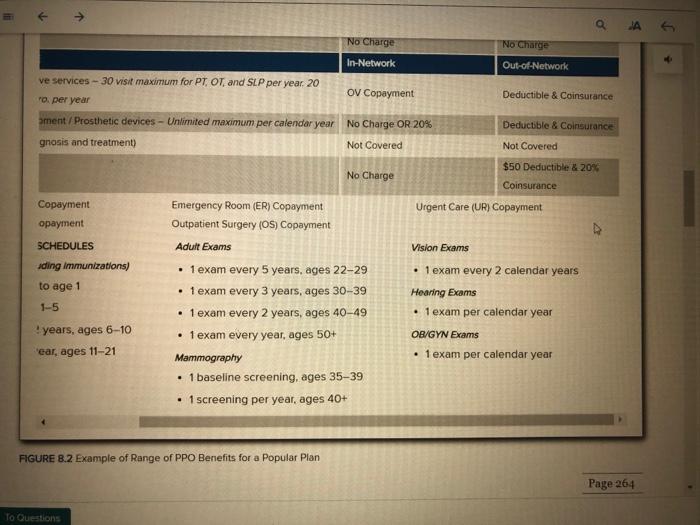
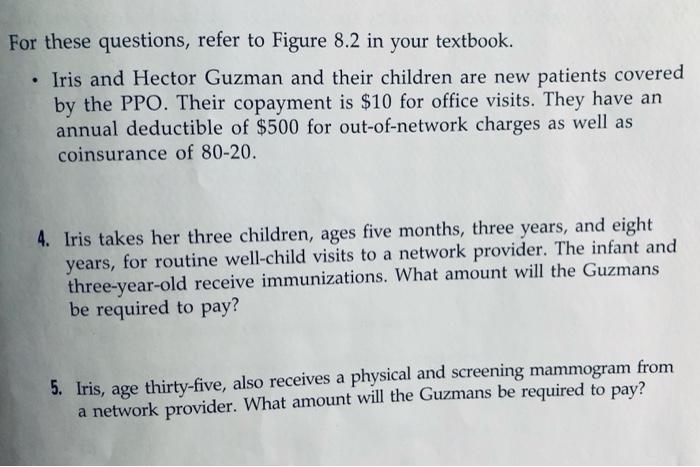
Concepts Standard Benefits This is a preferred provider organization (PPO) plan. That means members can receive the highest level of benefits when they use any of the more than 5,000 physicians and other healthcare professionals in this network. When members receive covered in network services, they simply pay a copayment Members can also receive care from providers that are not part of the network however, benefits are often lower and covered claims are subject to deductible, coinsurance and charges above the maximum allowable amount Referrals are not needed from a Primary Care Physician to receive care from a specialist PREVENTIVE CARE In-Network Out Ded Well child care Birth through 12 years All others Periodic, routine health examinations Ded Ded Routine eye exams Ded OV Copayment OV Copayment OV Copayment Ov Copayment OV Copayment No Charge ovkopayment In-Network Ded Ded Ded Out Ded Routine OB/GYN visits Mammography Heating Screening MEDICAL CARE PCP office visits Specialist office Visits Outpatient mental health & substance abuse - pro authorization required Maternity care-ital visit tyect to copayment no charge thereafter Diagnostic lab X-ray and testing Ded OV Copayment Ov Copayment OV Copayment ON Copayment No Charge Ded Ded Ded To Questions 2021 MAR IT a A G Dedi High-cost outpatient diagnostics - prior authorization required. The following are No Charge OR $200 Copayment Ded subject to copayment: MRI, MRA, CAT, CTA, PET, SPECT scans Allergy Services Office visits/testing O Copayment Ded Injections - 80 visits in 3 years $25 Copayment Ded: HOSPITAL CARE - Prlor authorization required In-Network Out Semi-private room (General Medical Surgical/Maternity) HSP Copayment Dedi Skilled nursing facility - up to 120 days per calendar year HSP Copayment Dedi Rehabilitative services - up to 60 days per calendar year No Charge Ded Outpatient surgery - in a hospital or surgical-center Os Copayment EMERGENCY CARE In-Network Out Walk-in centers O Copayment Dedi Urgent care centers - at participating centers only UR Copayment Not Emergency care - copayment waived if admitted ER Copayment ERC Ambulance No Charge No C OTHER HEALTHCARE In-Network Out- Outpatient rehabilitative services - 30 visit maximum for PT. OT and SLP per year 20 O Copayment Ded visit maximum for Chiro, per year Durable medical equipment/Prosthetic devices - Unlimited maximum per calendar year No Charge OR 20% Ded Infertility Services (diagnosis and treatment) Not Covered Not $50 Home Healthcare No Charge Coin To Questions = JA G Ded Durable medical equipment / Prosthetic devices - Unlimited maximum per calendar year No Charge OR 20% Infertility Services (diagnosis and treatment) Not Covered Not $50 Home Health Care No Charge Coin Urgent Care (UR) Copay KEY: Office Visit (OV) Copayment Hospital (HSP) Copayment Emergency Room (ER) Copayment Outpatient Surgery (OS) Copayment Adult Exams Vision Exams 1 exam every 2 cale Hearing Exams PREVENTIVE CARE SCHEDULES Welt Child Care including Immunizations 6 exams, birth to age 1 6 exams, ages 1-5 1 exam every 2 years, ages 6-10 1 exam every year, ages 11-21 1 exam per calende 1 exam every 5 years, ages 22-29 1 exam every 3 years, ages 30-39 1 exam every 2 years, ages 40-49 1 exam every year, ages 50+ Mammography 1 baseline screening, ages 35-39 1 screening per year, ages 40+ OB/GYN Exams 1 exam per calende FIGURE 8.2 Example of Range of PPO Benefits for a Popular Plan Page 264 BILLING TIP Private Payers To Questions Consumer-Driven Health Plan (Combined High-Deductible Health Plan and Funding Option) Up to Discounted Fee-for-Service Standard Benefits This is a preferred provider organization (PPO) plan. That means members can receive the highest level of benefits when they use any of the more than 5,000 physicians and other healthcare professionals in this network. When members receive covered in-network services, they simply pay a copayment. Members can also receive care from providers that are not part of the network, however, benefits are often lower and covered claims are subject to deductible, coinsurance and charges above the maximum allowable amount. Referrals are not needed from a Primary Care Physician to receive care from a specialist In-Network Out-of-Network h examinations OV Copayment OV Copayment OV Copayment Ov Copayment OV Copayment No Charge OV Copayment In-Network OV Copayment OV Copayment OV Copayment Deductible & Constance Deductible & Coinsurance Deductible & Coinsurance Deductible & Coinsurance Deductible & Coinsurance Deductible & Coinsurance Deductible & Coinsurance Out-of-Network Deductible & Coinsurance Deductible & Coinsurance Deductible & Coinsurance alth & substance abuse-prior authorization required Lo Questions OV Copayment Deductible & Coinsurance Deductible & Coinsurance Deductible & Coinsurance OV Copayment OV Copayment O Copayment No Charge uith & substance abuse-prior authorization required visit subject to copayment, no charge thereafter and testing diagnostics - prior authorization required. The following are MRI MRA, CAT, CTA, PET, SPECT scans Deductible & Coinsurance Deductible & Coinsurance No Charge OR $200 Copayment Deductible & Coinsurance n 3 years or authorization required eneral Medical Surgical Maternity) up to 120 days per calendar year 1 - up to 60 days per calendar year na hospital or surgical-center OV Copayment $25 Copayment In-Network HSP Copayment HSP Copayment No Charge Os Copayment In-Network Ov Copayment UR Copayment ER Copayment No Charge Deductible & Coinsurance Deductible & Coinsurance Out-of-Network Deductible & Coinsurance Deductible & Coinsurance Deductible & Coinsurance Deductible & Coinsurance Out-of-Network Deductible & Coinsurance Not Covered at participating centers only ER Copayment payment waived if admitted No Charge In-Network Out-of-Network amavimmar DTOT ACID Radar an o Questions No Charge No Charge In-Network Out-of-Network Deductible & Coinsurance ve services - 30 visit maximum for PT, OT, and SLP per year. 20 OV Copayment To per year ament/Prosthetic devices - Unlimited maximum per calendar year No Charge OR 20% gnosis and treatment) Not Covered Deductible & Coinsurance Not Covered $50 Deductible & 20% No Charge Coinsurance Copayment opayment Urgent Care (UR) Copayment Emergency Room (ER) Copayment Outpatient Surgery (OS) Copayment Adult Exams Vision Exams SCHEDULES ding Immunizations) to age 1 1-5 . 1 exam every 5 years, ages 22-29 1 exam every 3 years, ages 30-39 1 exam every 2 years, ages 40-49 1exam every year, ages 50+ Mammography 1 baseline screening, ages 35-39 1 screening per year, ages 40+ 1 exam every 2 calendar years Hearing Exams 1 exam per calendar year OB/GYN Exams 1 exam per calendar year years, ages 6-10 ear, ages 11-21 FIGURE 8.2 Example of Range of PPO Benefits for a Popular Plan Page 264 To Questions For these questions, refer to Figure 8.2 in your textbook. Iris and Hector Guzman and their children are new patients covered by the PPO. Their copayment is $10 for office visits. They have an annual deductible of $500 for out-of-network charges as well as coinsurance of 80-20. 4. Iris takes her three children, ages five months, three years, and eight years, for routine well-child visits to a network provider. The infant and three-year-old receive immunizations. What amount will the Guzmans be required to pay? 5. Iris, age thirty-five, also receives a physical and screening mammogram from a network provider. What amount will the Guzmans be required to pay? Concepts Standard Benefits This is a preferred provider organization (PPO) plan. That means members can receive the highest level of benefits when they use any of the more than 5,000 physicians and other healthcare professionals in this network. When members receive covered in network services, they simply pay a copayment Members can also receive care from providers that are not part of the network however, benefits are often lower and covered claims are subject to deductible, coinsurance and charges above the maximum allowable amount Referrals are not needed from a Primary Care Physician to receive care from a specialist PREVENTIVE CARE In-Network Out Ded Well child care Birth through 12 years All others Periodic, routine health examinations Ded Ded Routine eye exams Ded OV Copayment OV Copayment OV Copayment Ov Copayment OV Copayment No Charge ovkopayment In-Network Ded Ded Ded Out Ded Routine OB/GYN visits Mammography Heating Screening MEDICAL CARE PCP office visits Specialist office Visits Outpatient mental health & substance abuse - pro authorization required Maternity care-ital visit tyect to copayment no charge thereafter Diagnostic lab X-ray and testing Ded OV Copayment Ov Copayment OV Copayment ON Copayment No Charge Ded Ded Ded To Questions 2021 MAR IT a A G Dedi High-cost outpatient diagnostics - prior authorization required. The following are No Charge OR $200 Copayment Ded subject to copayment: MRI, MRA, CAT, CTA, PET, SPECT scans Allergy Services Office visits/testing O Copayment Ded Injections - 80 visits in 3 years $25 Copayment Ded: HOSPITAL CARE - Prlor authorization required In-Network Out Semi-private room (General Medical Surgical/Maternity) HSP Copayment Dedi Skilled nursing facility - up to 120 days per calendar year HSP Copayment Dedi Rehabilitative services - up to 60 days per calendar year No Charge Ded Outpatient surgery - in a hospital or surgical-center Os Copayment EMERGENCY CARE In-Network Out Walk-in centers O Copayment Dedi Urgent care centers - at participating centers only UR Copayment Not Emergency care - copayment waived if admitted ER Copayment ERC Ambulance No Charge No C OTHER HEALTHCARE In-Network Out- Outpatient rehabilitative services - 30 visit maximum for PT. OT and SLP per year 20 O Copayment Ded visit maximum for Chiro, per year Durable medical equipment/Prosthetic devices - Unlimited maximum per calendar year No Charge OR 20% Ded Infertility Services (diagnosis and treatment) Not Covered Not $50 Home Healthcare No Charge Coin To Questions = JA G Ded Durable medical equipment / Prosthetic devices - Unlimited maximum per calendar year No Charge OR 20% Infertility Services (diagnosis and treatment) Not Covered Not $50 Home Health Care No Charge Coin Urgent Care (UR) Copay KEY: Office Visit (OV) Copayment Hospital (HSP) Copayment Emergency Room (ER) Copayment Outpatient Surgery (OS) Copayment Adult Exams Vision Exams 1 exam every 2 cale Hearing Exams PREVENTIVE CARE SCHEDULES Welt Child Care including Immunizations 6 exams, birth to age 1 6 exams, ages 1-5 1 exam every 2 years, ages 6-10 1 exam every year, ages 11-21 1 exam per calende 1 exam every 5 years, ages 22-29 1 exam every 3 years, ages 30-39 1 exam every 2 years, ages 40-49 1 exam every year, ages 50+ Mammography 1 baseline screening, ages 35-39 1 screening per year, ages 40+ OB/GYN Exams 1 exam per calende FIGURE 8.2 Example of Range of PPO Benefits for a Popular Plan Page 264 BILLING TIP Private Payers To Questions Consumer-Driven Health Plan (Combined High-Deductible Health Plan and Funding Option) Up to Discounted Fee-for-Service Standard Benefits This is a preferred provider organization (PPO) plan. That means members can receive the highest level of benefits when they use any of the more than 5,000 physicians and other healthcare professionals in this network. When members receive covered in-network services, they simply pay a copayment. Members can also receive care from providers that are not part of the network, however, benefits are often lower and covered claims are subject to deductible, coinsurance and charges above the maximum allowable amount. Referrals are not needed from a Primary Care Physician to receive care from a specialist In-Network Out-of-Network h examinations OV Copayment OV Copayment OV Copayment Ov Copayment OV Copayment No Charge OV Copayment In-Network OV Copayment OV Copayment OV Copayment Deductible & Constance Deductible & Coinsurance Deductible & Coinsurance Deductible & Coinsurance Deductible & Coinsurance Deductible & Coinsurance Deductible & Coinsurance Out-of-Network Deductible & Coinsurance Deductible & Coinsurance Deductible & Coinsurance alth & substance abuse-prior authorization required Lo Questions OV Copayment Deductible & Coinsurance Deductible & Coinsurance Deductible & Coinsurance OV Copayment OV Copayment O Copayment No Charge uith & substance abuse-prior authorization required visit subject to copayment, no charge thereafter and testing diagnostics - prior authorization required. The following are MRI MRA, CAT, CTA, PET, SPECT scans Deductible & Coinsurance Deductible & Coinsurance No Charge OR $200 Copayment Deductible & Coinsurance n 3 years or authorization required eneral Medical Surgical Maternity) up to 120 days per calendar year 1 - up to 60 days per calendar year na hospital or surgical-center OV Copayment $25 Copayment In-Network HSP Copayment HSP Copayment No Charge Os Copayment In-Network Ov Copayment UR Copayment ER Copayment No Charge Deductible & Coinsurance Deductible & Coinsurance Out-of-Network Deductible & Coinsurance Deductible & Coinsurance Deductible & Coinsurance Deductible & Coinsurance Out-of-Network Deductible & Coinsurance Not Covered at participating centers only ER Copayment payment waived if admitted No Charge In-Network Out-of-Network amavimmar DTOT ACID Radar an o Questions No Charge No Charge In-Network Out-of-Network Deductible & Coinsurance ve services - 30 visit maximum for PT, OT, and SLP per year. 20 OV Copayment To per year ament/Prosthetic devices - Unlimited maximum per calendar year No Charge OR 20% gnosis and treatment) Not Covered Deductible & Coinsurance Not Covered $50 Deductible & 20% No Charge Coinsurance Copayment opayment Urgent Care (UR) Copayment Emergency Room (ER) Copayment Outpatient Surgery (OS) Copayment Adult Exams Vision Exams SCHEDULES ding Immunizations) to age 1 1-5 . 1 exam every 5 years, ages 22-29 1 exam every 3 years, ages 30-39 1 exam every 2 years, ages 40-49 1exam every year, ages 50+ Mammography 1 baseline screening, ages 35-39 1 screening per year, ages 40+ 1 exam every 2 calendar years Hearing Exams 1 exam per calendar year OB/GYN Exams 1 exam per calendar year years, ages 6-10 ear, ages 11-21 FIGURE 8.2 Example of Range of PPO Benefits for a Popular Plan Page 264 To Questions For these questions, refer to Figure 8.2 in your textbook. Iris and Hector Guzman and their children are new patients covered by the PPO. Their copayment is $10 for office visits. They have an annual deductible of $500 for out-of-network charges as well as coinsurance of 80-20. 4. Iris takes her three children, ages five months, three years, and eight years, for routine well-child visits to a network provider. The infant and three-year-old receive immunizations. What amount will the Guzmans be required to pay? 5. Iris, age thirty-five, also receives a physical and screening mammogram from a network provider. What amount will the Guzmans be required to pay