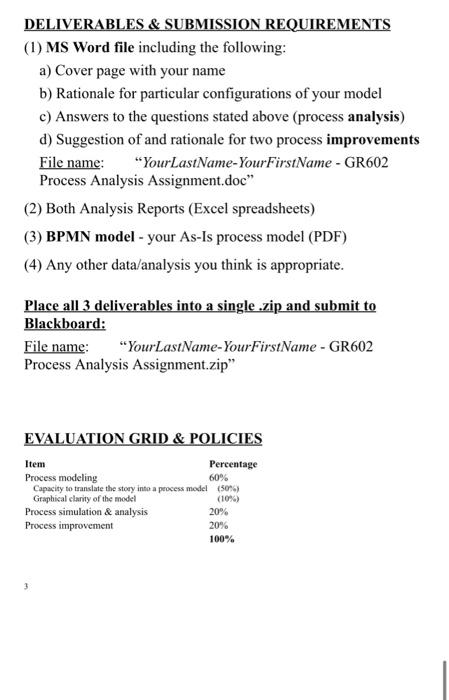
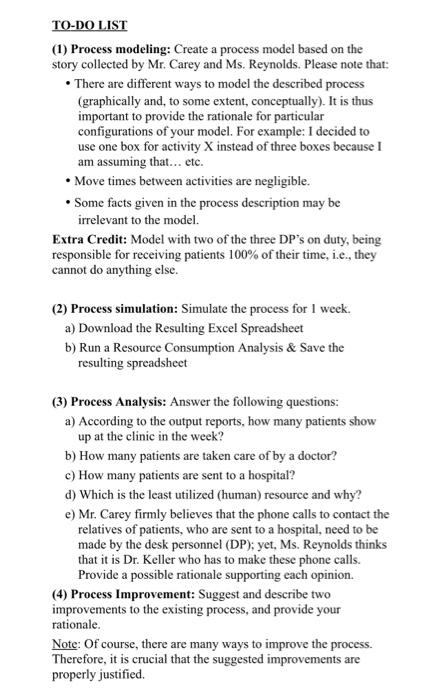
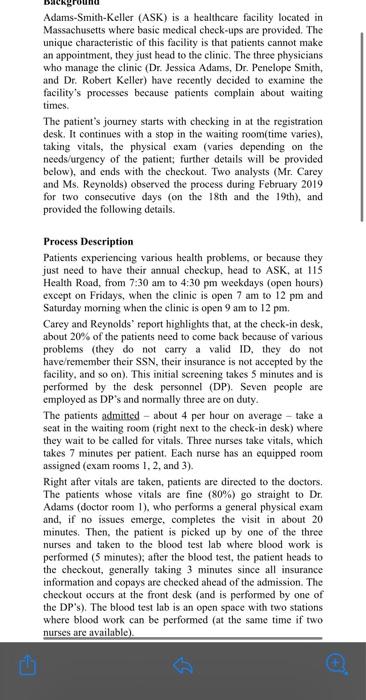
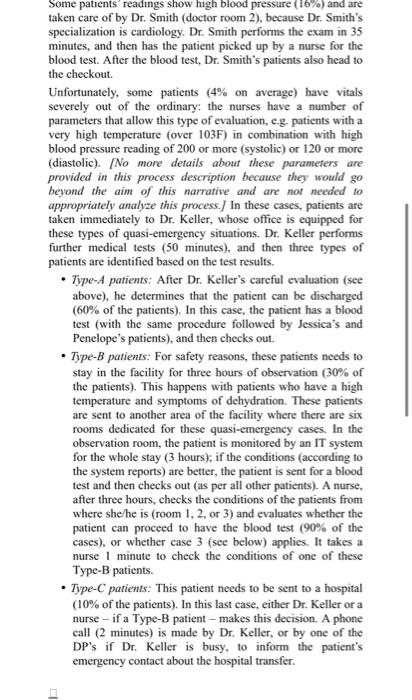
DELIVERABLES \& SUBMISSION REQUIREMENTS (1) MS Word file including the following: a) Cover page with your name b) Rationale for particular configurations of your model c) Answers to the questions stated above (process analysis) d) Suggestion of and rationale for two process improvements File name: "YourLastName-YourFirstName-GR602 Process Analysis Assignment.doc" (2) Both Analysis Reports (Excel spreadsheets) (3) BPMN model - your As-Is process model (PDF) (4) Any other data/analysis you think is appropriate. Place all 3 deliverables into a single .aip and submit to Blackboard: File name: "YourLastName-YourFirstName - GR602 Process Analysis Assignment.zip" EVALUATION GRID \& POLICIES TO-DO LIST (1) Process modeling: Create a process model based on the story collected by Mr. Carey and Ms. Reynolds. Please note that: - There are different ways to model the described process (graphically and, to some extent, conceptually). It is thus important to provide the rationale for particular configurations of your model. For example: I decided to use one box for activity X instead of three boxes because I am assuming that... etc. - Move times between activities are negligible. - Some facts given in the process description may be irrelevant to the model. Extra Credit: Model with two of the three DP's on duty, being responsible for receiving patients 100% of their time, i.e., they cannot do anything else. (2) Process simulation: Simulate the process for 1 week. a) Download the Resulting Excel Spreadsheet b) Run a Resource Consumption Analysis \& Save the resulting spreadsheet (3) Process Analysis: Answer the following questions: a) According to the output reports, how many patients show up at the clinic in the week? b) How many patients are taken care of by a doctor? c) How many patients are sent to a hospital? d) Which is the least utilized (human) resource and why? e) Mr. Carey firmly believes that the phone calls to contact the relatives of patients, who are sent to a hospital, need to be made by the desk personnel (DP); yet, Ms. Reynolds thinks that it is Dr. Keller who has to make these phone calls. Provide a possible rationale supporting each opinion. (4) Process Improvement: Suggest and describe two improvements to the existing process, and provide your rationale. Note: Of course, there are many ways to improve the process. Therefore, it is crucial that the suggested improvements are properly justified. Adams-Smith-Keller (ASK) is a healthcare facility located in Massachusetts where basic medical check-ups are provided. The unique characteristic of this facility is that patients cannot make an appointment, they just head to the elinic. The three physicians who manage the clinic (Dr. Jessica Adams, Dr. Penelope Smith, and Dr. Robert Keller) have recently decided to examine the facility's processes because patients complain about waiting times. The patient's journey starts with checking in at the registration desk. It continues with a stop in the waiting room(time varies), taking vitals, the physical exam (varies depending on the needs/urgency of the patient; further details will be provided below), and ends with the checkout. Two analysts (Mr. Carey and Ms. Reynolds) observed the process during February 2019 for two consecutive days (on the 18 th and the 19th), and provided the following details. Process Description Patients experiencing various health problems, or because they just need to have their annual checkup, head to ASK, at 115 Health Road, from 7:30 am to 4:30pm weekdays (open hours) except on Fridays, when the clinic is open 7 am to 12pm and Saturday morning when the clinic is open 9 am to 12pm. Carey and Reynolds' report highlights that, at the check-in desk, about 20% of the patients need to come back because of various problems (they do not carry a valid ID, they do not have/remember their SSN, their insurance is not accepted by the facility, and so on). This initial sereening takes 5 minutes and is performed by the desk personnel (DP). Seven people are employed as DP's and normally three are on duty. The patients admitted - about 4 per hour on average - take a seat in the waiting room (right next to the check-in desk) where they wait to be called for vitals. Three nurses take vitals, which takes 7 minutes per patient. Each nurse has an equipped room assigned (exam rooms 1,2, and 3). Right after vitals are taken, patients are directed to the doctors. The patients whose vitals are fine (80%) go straight to Dr. Adams (doctor room 1), who performs a general physical exam and, if no issues emerge, completes the visit in about 20 minutes. Then, the patient is picked up by one of the three nurses and taken to the blood test lab where blood work is performed ( 5 minutes); after the blood test, the patient heads to the checkout, generally taking 3 minutes since all insurance information and copays are checked ahead of the admission. The checkout occurs at the front desk (and is performed by one of the DP's). The blood test lab is an open space with two stations where blood work can be performed (at the same time if two nurses are available). Some patients' readings show high blood pressure (16%) and are taken care of by Dr. Smith (doctor room 2), because Dr. Smith's specialization is cardiology. Dr. Smith performs the exam in 35 minutes, and then has the patient picked up by a nurse for the blood test. After the blood test, Dr. Smith's patients also head to the checkout. Unfortunately, some patients (4\% on average) have vitals severely out of the ordinary: the nurses have a number of parameters that allow this type of evaluation, eg. patients with a very high temperature (over 103F) in combination with high blood pressure reading of 200 or more (systolic) or 120 or more (diastolic). [No more details about these parameters are provided in this process description because they would go beyond the aim of this narrative and are not needed to appropriately analyze this process.J In these cases, patients are taken immediately to Dr. Keller, whose office is equipped for these types of quasi-emergency situations. Dr. Keller performs further medical tests ( 50 minutes), and then three types of patients are identified based on the test results. - Type-A patients: After Dr. Keller's careful evaluation (see above), he determines that the patient can be discharged ( 60% of the patients). In this case, the patient has a blood test (with the same procedure followed by Jessica's and Penelope's patients), and then checks out. - Type-B patients: For safety reasons, these patients needs to stay in the facility for three hours of observation ( 30% of the patients). This happens with patients who have a high temperature and symptoms of dehydration. These patients are sent to another area of the facility where there are six rooms dedicated for these quasi-emergency cases. In the observation room, the patient is monitored by an IT system for the whole stay (3 hours); if the conditions (according to the system reports) are better, the patient is sent for a blood test and then checks out (as per all other patients). A nurse, after three hours, checks the conditions of the patients from where she/he is (room 1, 2, or 3) and evaluates whether the patient can proceed to have the blood test ( 90% of the cases), or whether case 3 (see below) applies. It takes a nurse I minute to check the conditions of one of these Type-B patients. - Type-C patients: This patient needs to be sent to a hospital ( 10% of the patients). In this last case, either Dr. Keller or a nurse - if a Type-B patient - makes this decision. A phone call ( 2 minutes) is made by Dr. Keller, or by one of the DP's if Dr. Keller is busy, to inform the patient's emergency contact about the hospital transfer. Adams-Smith-Keller (ASK) is a healtheare facility located in Massachusetts where basic medical check-ups are provided. The unique characteristic of this facility is that patients cannot make an appointment, they just head to the clinic. The three physicians who manage the clinic (Dr. Jessica Adams, Dr. Penelope Smith, and Dr. Robert Keller) have recently decided to examine the facility's processes because patients complain about waiting times. The patient's journey starts with checking in at the registration desk. It continues with a stop in the waiting room(time varies). taking vitals, the physical exam (varies depending on the needs/urgency of the patient; further details will be provided below), and ends with the checkout. Two analysts (Mr. Carey and Ms. Reynolds) observed the process during February 2019 for two consecutive days (on the 18 th and the 19th), and provided the following details. Some pattents readings show high blood pressure (16%) and are taken care of by Dr. Smith (doctor room 2), because Dr. Smith's specialization is cardiology. Dr. Smith performs the exam in 35 minutes, and then has the patient picked up by a nurse for the blood test. After the blood test, Dr. Smith's patients also head to the checkout. Unfortunately, some patients ( 4% on average) have vitals severely out of the ordinary: the nurses have a number of parameters that allow this type of evaluation, e.g. patients with a very high temperature (over 103F) in combination with high blood pressure reading of 200 or more (systolic) or 120 or more (diastolic). [No more details about these parameters are provided in this process description because they would go beyond the aim of this narrative and are not needed to appropriately analyze this process. I In these cases, patients are taken immediately to Dr. Keller, whose office is equipped for these types of quasi-emergency situations. Dr. Keller performs patients are identified based on the test results. - Type-A patients: After Dr. Keller's careful evaluation (see above), he determines that the patient can be discharged (60% of the patients). In this case, the patient has a blood test (with the same procedure followed by Jessica's and Penelope's patients), and then checks out. - Type-B patients: For safety reasons, these patients needs to stay in the facility for three hours of observation ( 30% of the patients). This happens with patients who have a high temperature and symptoms of dehydration. These patients are sent to another area of the facility where there are six rooms dedicated for these quasi-emergency cases. In the observation room, the patient is monitored by an IT system for the whole stay ( 3 hours); if the conditions (according to the system reports) are better, the patient is sent for a blood test and then checks out (as per all other patients). A nurse, after three hours, checks the conditions of the patients from where she/he is (room 1,2, or 3) and evaluates whether the patient can proceed to have the blood test (90% of the cases), or whether case 3 (see below) applies. It takes a nurse 1 minute to check the conditions of one of these Type-B patients. - Type-C patients: This patient needs to be sent to a hospital ( 10% of the patients). In this last case, either Dr. Keller or a nurse - if a Type-B patient - makes this decision. A phone call ( 2 minutes) is made by Dr. Keller, or by one of the DP's if Dr. Keller is busy, to inform the patient's emergency contact about the hospital transfer. DELIVERABLES \& SUBMISSION REQUIREMENTS (1) MS Word file including the following: a) Cover page with your name b) Rationale for particular configurations of your model c) Answers to the questions stated above (process analysis) d) Suggestion of and rationale for two process improvements File name: "YourLastName-YourFirstName - GR602 Process Analysis Assignment.doc" (2) Both Analysis Reports (Excel spreadsheets) (3) BPMN model - your As-Is process model (PDF) (4) Any other data/analysis you think is appropriate. TO-DO LIST (1) Process modeling: Create a process model based on the story collected by Mr. Carey and Ms. Reynolds. Please note that: - There are different ways to model the described process (graphically and, to some extent, conceptually). It is thus important to provide the rationale for particular configurations of your model. For example: I decided to use one box for activity X instead of three boxes because I am assuming that... etc. - Move times between activities are negligible. - Some facts given in the process description may be irrelevant to the model. Extra Credit: Model with two of the three DP's on duty, being responsible for receiving patients 100% of their time, i.e., they cannot do anything else. (2) Process simulation: Simulate the process for 1 week. a) Download the Resulting Excel Spreadsheet b) Run a Resource Consumption Analysis \& Save the resulting spreadsheet (3) Process Analysis: Answer the following questions: a) According to the output reports, how many patients show up at the clinic in the week? b) How many patients are taken care of by a doctor? c) How many patients are sent to a hospital? d) Which is the least utilized (human) resource and why? e) Mr. Carey firmly believes that the phone calls to contact the relatives of patients, who are sent to a hospital, need to be made by the desk personnel (DP); yet, Ms. Reynolds thinks that it is Dr. Keller who has to make these phone calls. Provide a possible rationale supporting each opinion. (4) Process Improvement: Suggest and describe two improvements to the existing process, and provide your rationale. Note: Of course, there are many ways to improve the process. Therefore, it is crucial that the suggested improvements are properly justified. DELIVERABLES \& SUBMISSION REQUIREMENTS (1) MS Word file including the following: a) Cover page with your name b) Rationale for particular configurations of your model c) Answers to the questions stated above (process analysis) d) Suggestion of and rationale for two process improvements File name: "YourLastName-YourFirstName-GR602 Process Analysis Assignment.doc" (2) Both Analysis Reports (Excel spreadsheets) (3) BPMN model - your As-Is process model (PDF) (4) Any other data/analysis you think is appropriate. Place all 3 deliverables into a single .aip and submit to Blackboard: File name: "YourLastName-YourFirstName - GR602 Process Analysis Assignment.zip" EVALUATION GRID \& POLICIES TO-DO LIST (1) Process modeling: Create a process model based on the story collected by Mr. Carey and Ms. Reynolds. Please note that: - There are different ways to model the described process (graphically and, to some extent, conceptually). It is thus important to provide the rationale for particular configurations of your model. For example: I decided to use one box for activity X instead of three boxes because I am assuming that... etc. - Move times between activities are negligible. - Some facts given in the process description may be irrelevant to the model. Extra Credit: Model with two of the three DP's on duty, being responsible for receiving patients 100% of their time, i.e., they cannot do anything else. (2) Process simulation: Simulate the process for 1 week. a) Download the Resulting Excel Spreadsheet b) Run a Resource Consumption Analysis \& Save the resulting spreadsheet (3) Process Analysis: Answer the following questions: a) According to the output reports, how many patients show up at the clinic in the week? b) How many patients are taken care of by a doctor? c) How many patients are sent to a hospital? d) Which is the least utilized (human) resource and why? e) Mr. Carey firmly believes that the phone calls to contact the relatives of patients, who are sent to a hospital, need to be made by the desk personnel (DP); yet, Ms. Reynolds thinks that it is Dr. Keller who has to make these phone calls. Provide a possible rationale supporting each opinion. (4) Process Improvement: Suggest and describe two improvements to the existing process, and provide your rationale. Note: Of course, there are many ways to improve the process. Therefore, it is crucial that the suggested improvements are properly justified. Adams-Smith-Keller (ASK) is a healthcare facility located in Massachusetts where basic medical check-ups are provided. The unique characteristic of this facility is that patients cannot make an appointment, they just head to the elinic. The three physicians who manage the clinic (Dr. Jessica Adams, Dr. Penelope Smith, and Dr. Robert Keller) have recently decided to examine the facility's processes because patients complain about waiting times. The patient's journey starts with checking in at the registration desk. It continues with a stop in the waiting room(time varies), taking vitals, the physical exam (varies depending on the needs/urgency of the patient; further details will be provided below), and ends with the checkout. Two analysts (Mr. Carey and Ms. Reynolds) observed the process during February 2019 for two consecutive days (on the 18 th and the 19th), and provided the following details. Process Description Patients experiencing various health problems, or because they just need to have their annual checkup, head to ASK, at 115 Health Road, from 7:30 am to 4:30pm weekdays (open hours) except on Fridays, when the clinic is open 7 am to 12pm and Saturday morning when the clinic is open 9 am to 12pm. Carey and Reynolds' report highlights that, at the check-in desk, about 20% of the patients need to come back because of various problems (they do not carry a valid ID, they do not have/remember their SSN, their insurance is not accepted by the facility, and so on). This initial sereening takes 5 minutes and is performed by the desk personnel (DP). Seven people are employed as DP's and normally three are on duty. The patients admitted - about 4 per hour on average - take a seat in the waiting room (right next to the check-in desk) where they wait to be called for vitals. Three nurses take vitals, which takes 7 minutes per patient. Each nurse has an equipped room assigned (exam rooms 1,2, and 3). Right after vitals are taken, patients are directed to the doctors. The patients whose vitals are fine (80%) go straight to Dr. Adams (doctor room 1), who performs a general physical exam and, if no issues emerge, completes the visit in about 20 minutes. Then, the patient is picked up by one of the three nurses and taken to the blood test lab where blood work is performed ( 5 minutes); after the blood test, the patient heads to the checkout, generally taking 3 minutes since all insurance information and copays are checked ahead of the admission. The checkout occurs at the front desk (and is performed by one of the DP's). The blood test lab is an open space with two stations where blood work can be performed (at the same time if two nurses are available). Some patients' readings show high blood pressure (16%) and are taken care of by Dr. Smith (doctor room 2), because Dr. Smith's specialization is cardiology. Dr. Smith performs the exam in 35 minutes, and then has the patient picked up by a nurse for the blood test. After the blood test, Dr. Smith's patients also head to the checkout. Unfortunately, some patients (4\% on average) have vitals severely out of the ordinary: the nurses have a number of parameters that allow this type of evaluation, eg. patients with a very high temperature (over 103F) in combination with high blood pressure reading of 200 or more (systolic) or 120 or more (diastolic). [No more details about these parameters are provided in this process description because they would go beyond the aim of this narrative and are not needed to appropriately analyze this process.J In these cases, patients are taken immediately to Dr. Keller, whose office is equipped for these types of quasi-emergency situations. Dr. Keller performs further medical tests ( 50 minutes), and then three types of patients are identified based on the test results. - Type-A patients: After Dr. Keller's careful evaluation (see above), he determines that the patient can be discharged ( 60% of the patients). In this case, the patient has a blood test (with the same procedure followed by Jessica's and Penelope's patients), and then checks out. - Type-B patients: For safety reasons, these patients needs to stay in the facility for three hours of observation ( 30% of the patients). This happens with patients who have a high temperature and symptoms of dehydration. These patients are sent to another area of the facility where there are six rooms dedicated for these quasi-emergency cases. In the observation room, the patient is monitored by an IT system for the whole stay (3 hours); if the conditions (according to the system reports) are better, the patient is sent for a blood test and then checks out (as per all other patients). A nurse, after three hours, checks the conditions of the patients from where she/he is (room 1, 2, or 3) and evaluates whether the patient can proceed to have the blood test ( 90% of the cases), or whether case 3 (see below) applies. It takes a nurse I minute to check the conditions of one of these Type-B patients. - Type-C patients: This patient needs to be sent to a hospital ( 10% of the patients). In this last case, either Dr. Keller or a nurse - if a Type-B patient - makes this decision. A phone call ( 2 minutes) is made by Dr. Keller, or by one of the DP's if Dr. Keller is busy, to inform the patient's emergency contact about the hospital transfer. Adams-Smith-Keller (ASK) is a healtheare facility located in Massachusetts where basic medical check-ups are provided. The unique characteristic of this facility is that patients cannot make an appointment, they just head to the clinic. The three physicians who manage the clinic (Dr. Jessica Adams, Dr. Penelope Smith, and Dr. Robert Keller) have recently decided to examine the facility's processes because patients complain about waiting times. The patient's journey starts with checking in at the registration desk. It continues with a stop in the waiting room(time varies). taking vitals, the physical exam (varies depending on the needs/urgency of the patient; further details will be provided below), and ends with the checkout. Two analysts (Mr. Carey and Ms. Reynolds) observed the process during February 2019 for two consecutive days (on the 18 th and the 19th), and provided the following details. Some pattents readings show high blood pressure (16%) and are taken care of by Dr. Smith (doctor room 2), because Dr. Smith's specialization is cardiology. Dr. Smith performs the exam in 35 minutes, and then has the patient picked up by a nurse for the blood test. After the blood test, Dr. Smith's patients also head to the checkout. Unfortunately, some patients ( 4% on average) have vitals severely out of the ordinary: the nurses have a number of parameters that allow this type of evaluation, e.g. patients with a very high temperature (over 103F) in combination with high blood pressure reading of 200 or more (systolic) or 120 or more (diastolic). [No more details about these parameters are provided in this process description because they would go beyond the aim of this narrative and are not needed to appropriately analyze this process. I In these cases, patients are taken immediately to Dr. Keller, whose office is equipped for these types of quasi-emergency situations. Dr. Keller performs patients are identified based on the test results. - Type-A patients: After Dr. Keller's careful evaluation (see above), he determines that the patient can be discharged (60% of the patients). In this case, the patient has a blood test (with the same procedure followed by Jessica's and Penelope's patients), and then checks out. - Type-B patients: For safety reasons, these patients needs to stay in the facility for three hours of observation ( 30% of the patients). This happens with patients who have a high temperature and symptoms of dehydration. These patients are sent to another area of the facility where there are six rooms dedicated for these quasi-emergency cases. In the observation room, the patient is monitored by an IT system for the whole stay ( 3 hours); if the conditions (according to the system reports) are better, the patient is sent for a blood test and then checks out (as per all other patients). A nurse, after three hours, checks the conditions of the patients from where she/he is (room 1,2, or 3) and evaluates whether the patient can proceed to have the blood test (90% of the cases), or whether case 3 (see below) applies. It takes a nurse 1 minute to check the conditions of one of these Type-B patients. - Type-C patients: This patient needs to be sent to a hospital ( 10% of the patients). In this last case, either Dr. Keller or a nurse - if a Type-B patient - makes this decision. A phone call ( 2 minutes) is made by Dr. Keller, or by one of the DP's if Dr. Keller is busy, to inform the patient's emergency contact about the hospital transfer. DELIVERABLES \& SUBMISSION REQUIREMENTS (1) MS Word file including the following: a) Cover page with your name b) Rationale for particular configurations of your model c) Answers to the questions stated above (process analysis) d) Suggestion of and rationale for two process improvements File name: "YourLastName-YourFirstName - GR602 Process Analysis Assignment.doc" (2) Both Analysis Reports (Excel spreadsheets) (3) BPMN model - your As-Is process model (PDF) (4) Any other data/analysis you think is appropriate. TO-DO LIST (1) Process modeling: Create a process model based on the story collected by Mr. Carey and Ms. Reynolds. Please note that: - There are different ways to model the described process (graphically and, to some extent, conceptually). It is thus important to provide the rationale for particular configurations of your model. For example: I decided to use one box for activity X instead of three boxes because I am assuming that... etc. - Move times between activities are negligible. - Some facts given in the process description may be irrelevant to the model. Extra Credit: Model with two of the three DP's on duty, being responsible for receiving patients 100% of their time, i.e., they cannot do anything else. (2) Process simulation: Simulate the process for 1 week. a) Download the Resulting Excel Spreadsheet b) Run a Resource Consumption Analysis \& Save the resulting spreadsheet (3) Process Analysis: Answer the following questions: a) According to the output reports, how many patients show up at the clinic in the week? b) How many patients are taken care of by a doctor? c) How many patients are sent to a hospital? d) Which is the least utilized (human) resource and why? e) Mr. Carey firmly believes that the phone calls to contact the relatives of patients, who are sent to a hospital, need to be made by the desk personnel (DP); yet, Ms. Reynolds thinks that it is Dr. Keller who has to make these phone calls. Provide a possible rationale supporting each opinion. (4) Process Improvement: Suggest and describe two improvements to the existing process, and provide your rationale. Note: Of course, there are many ways to improve the process. Therefore, it is crucial that the suggested improvements are properly justified