Performing a case analysis on the American Heart Institute (AHI) within this case.

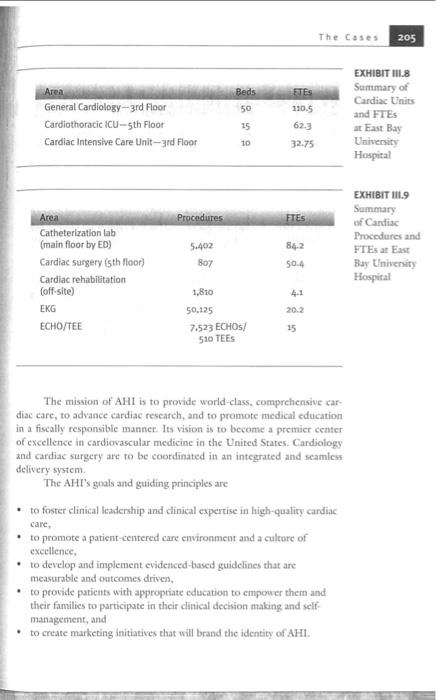
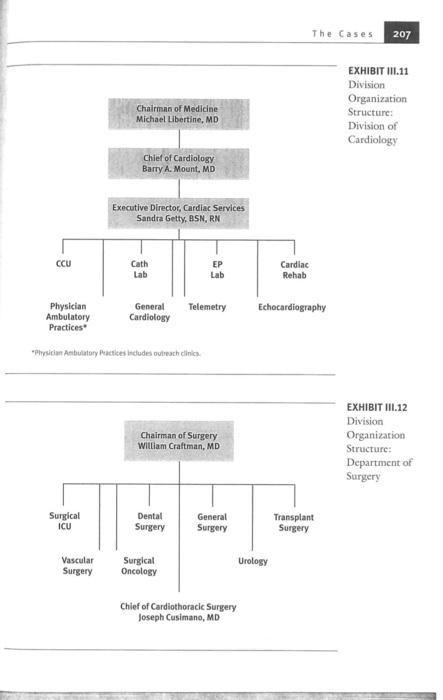
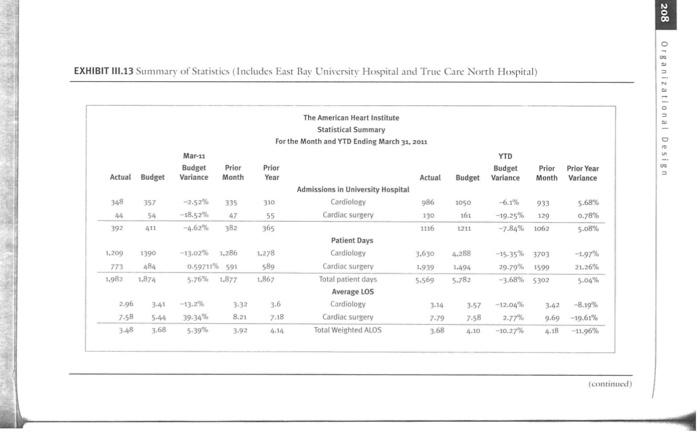
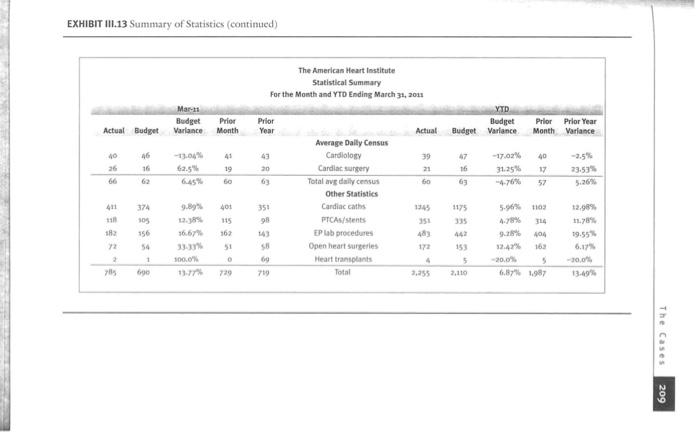
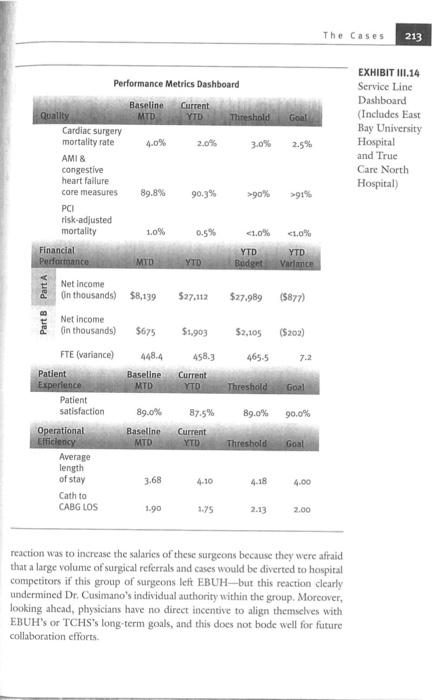
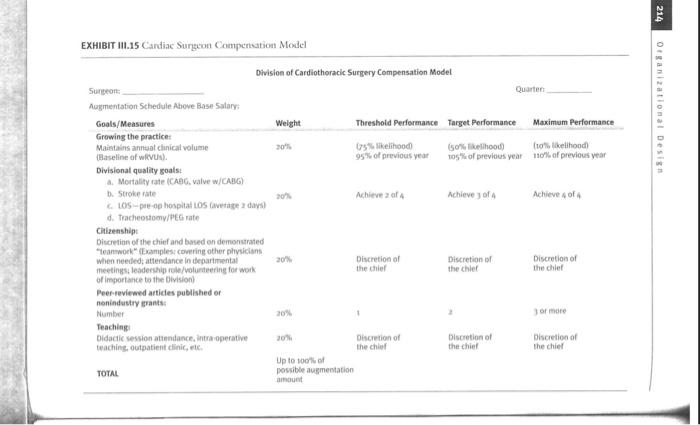
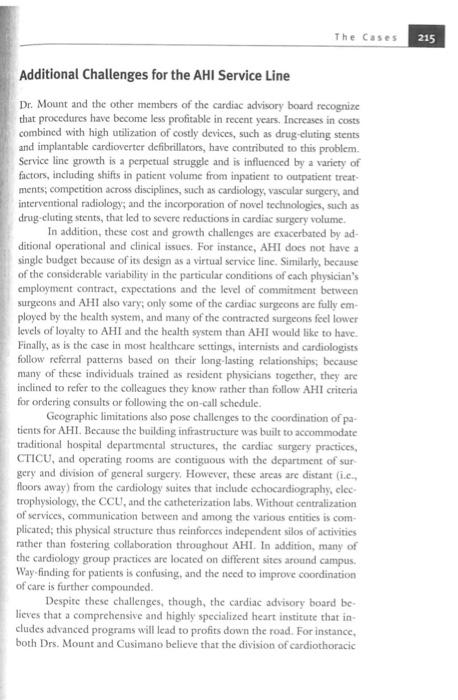
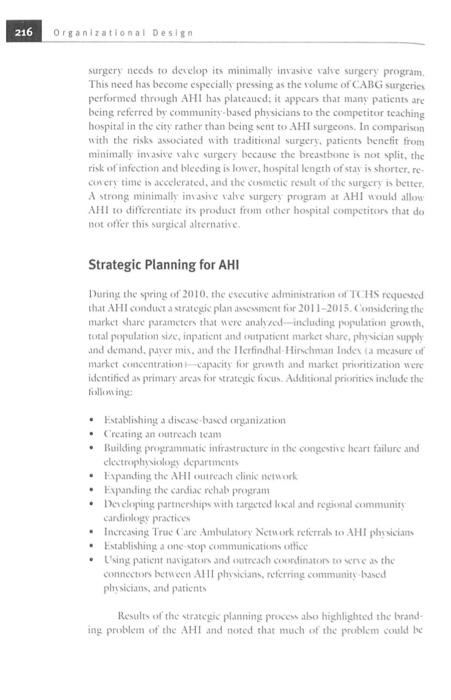
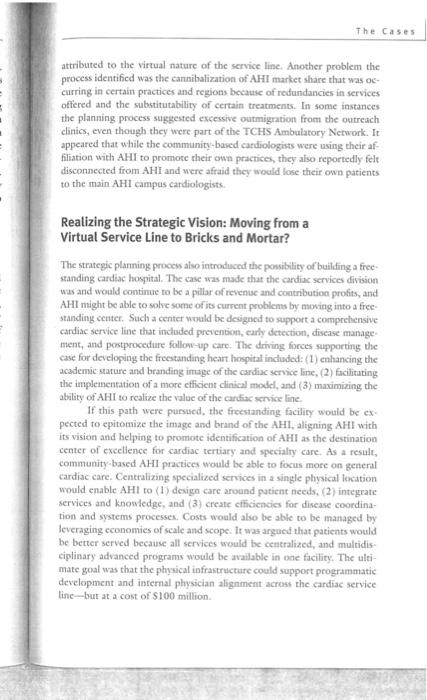
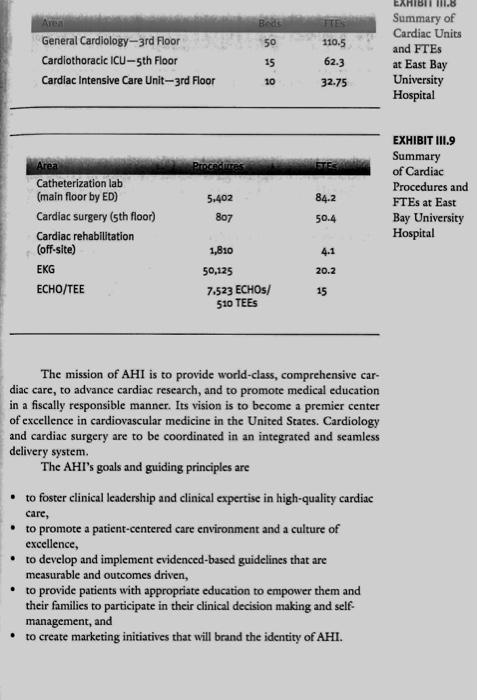
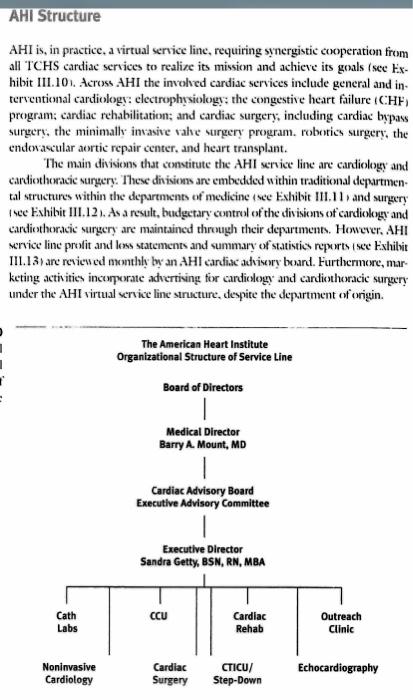
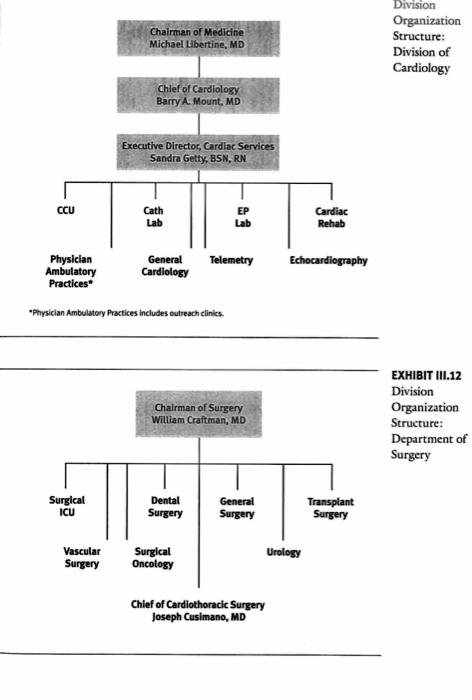
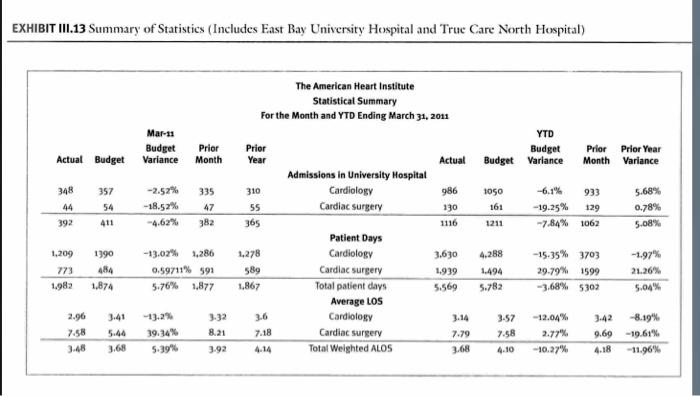
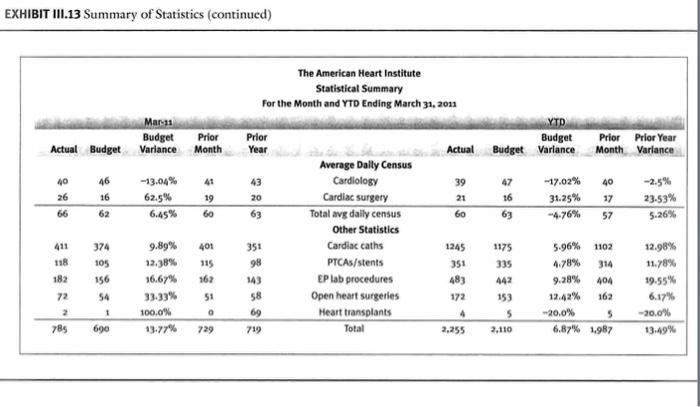
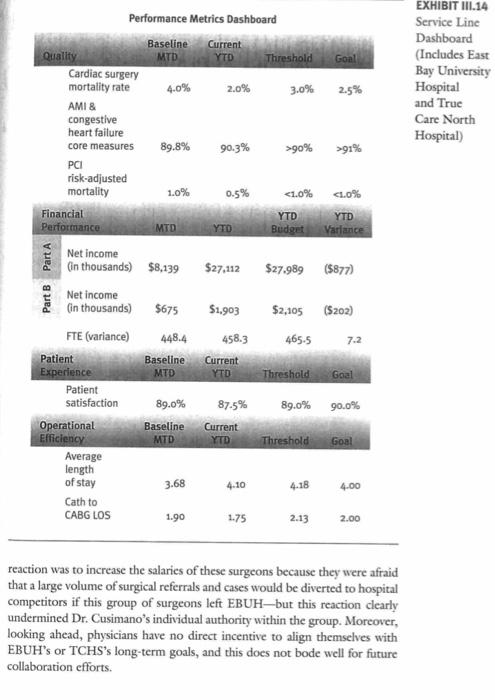
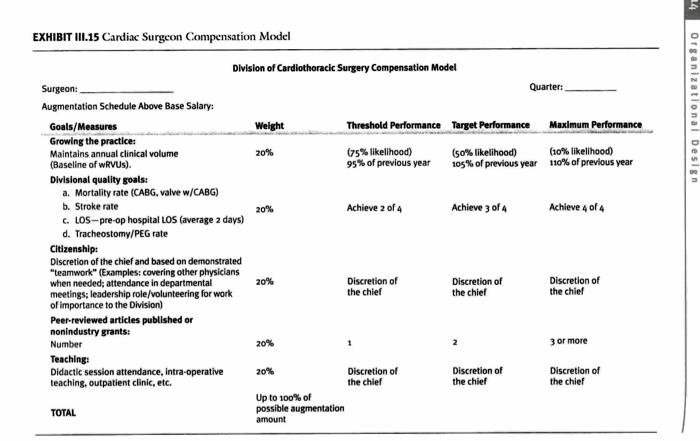
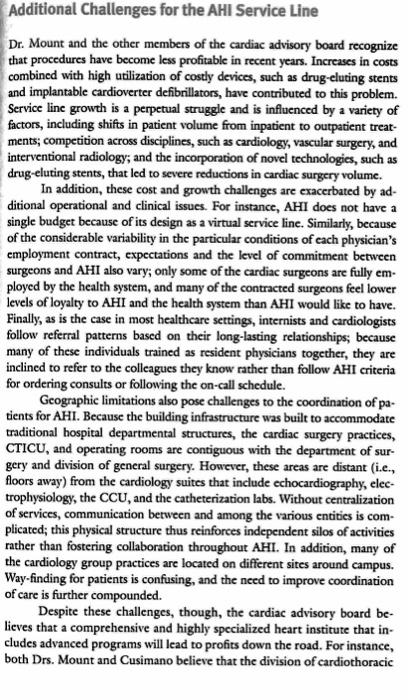
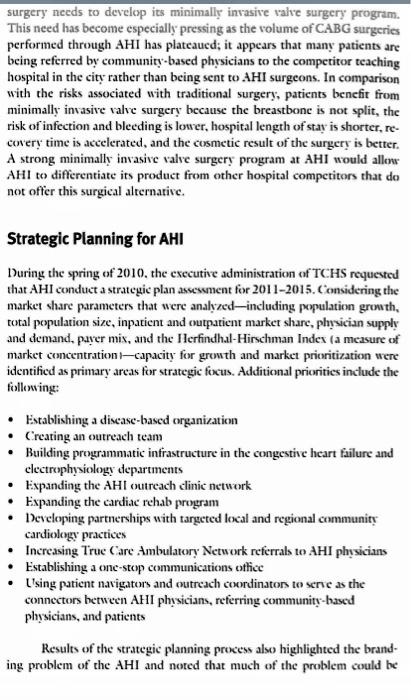
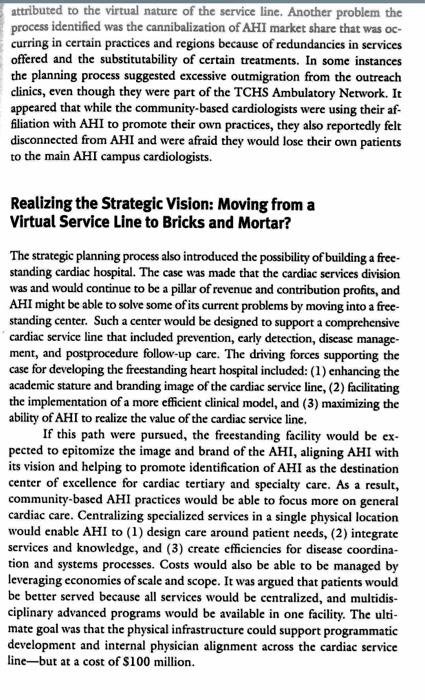
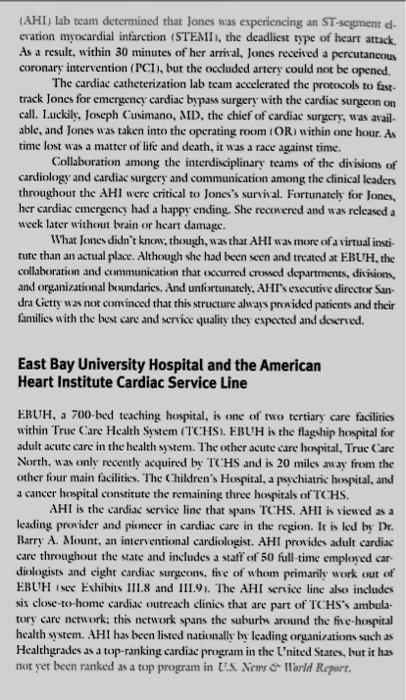
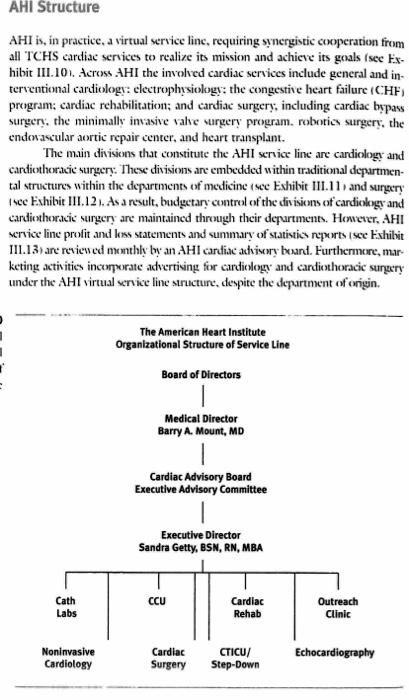
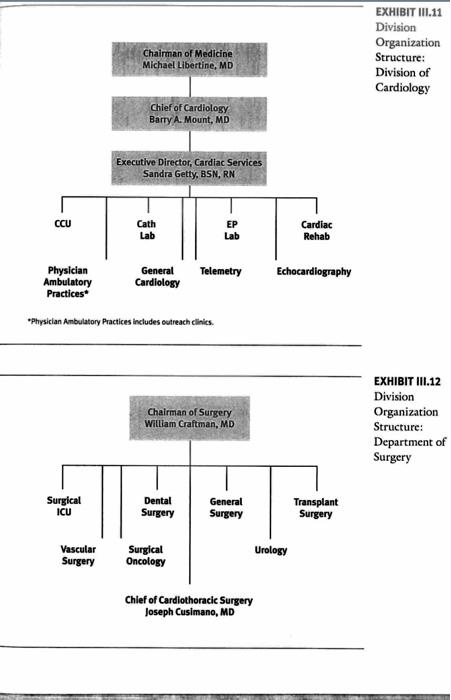
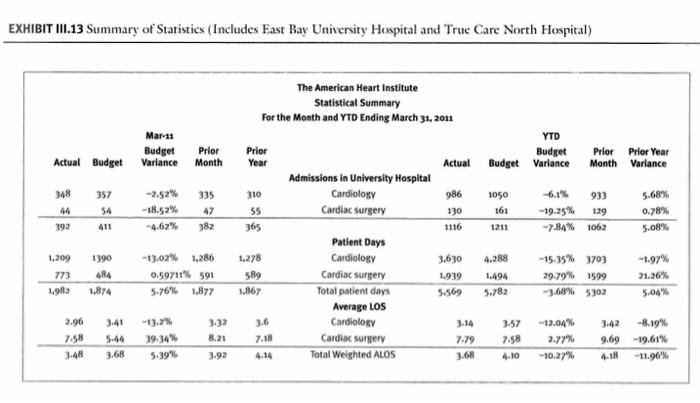
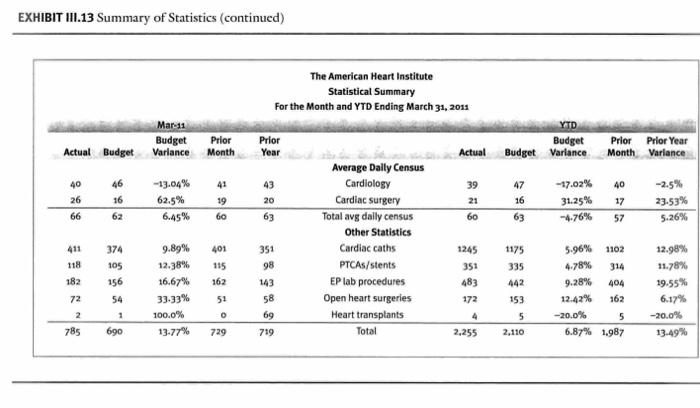
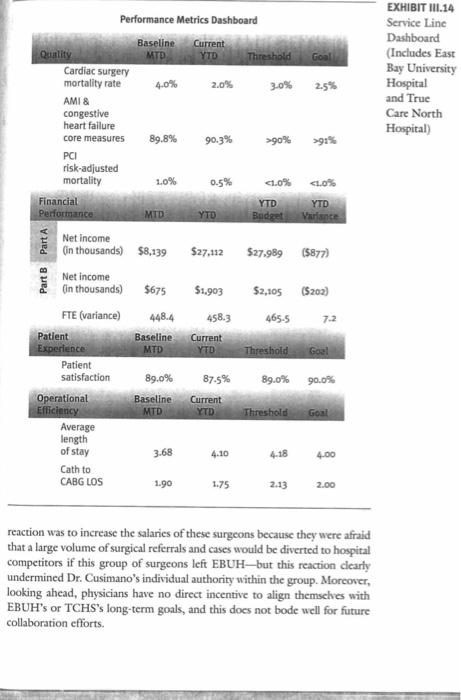
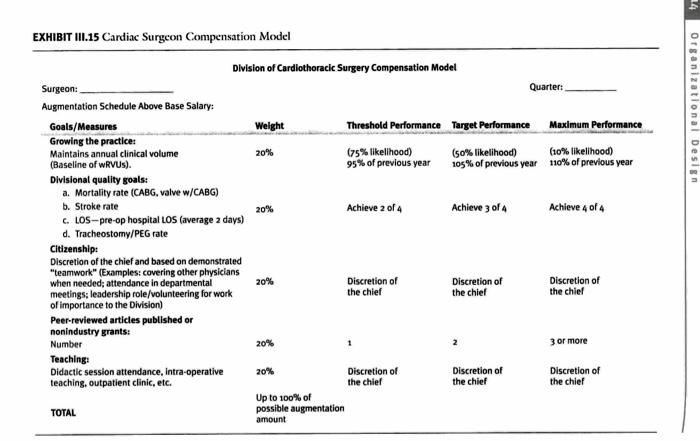
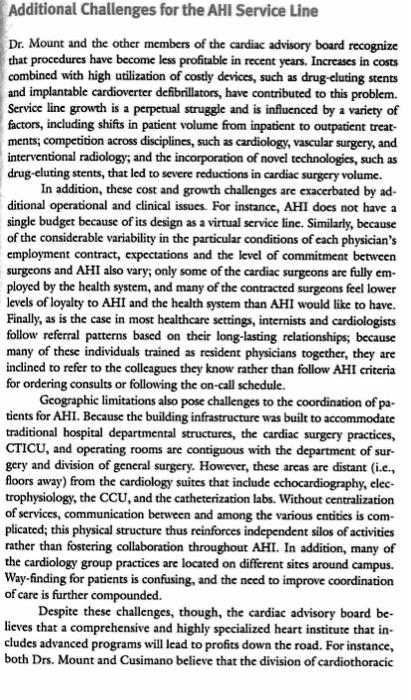
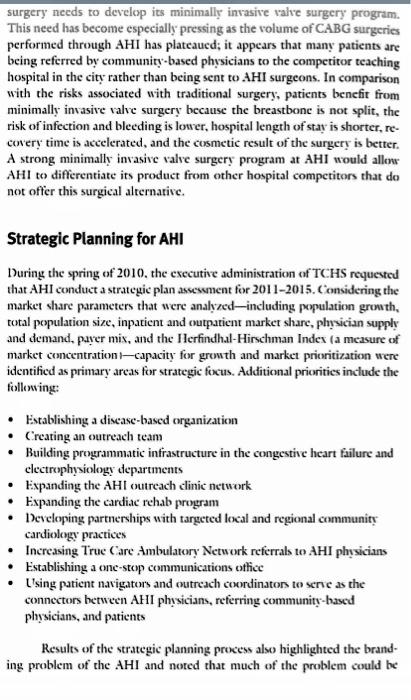
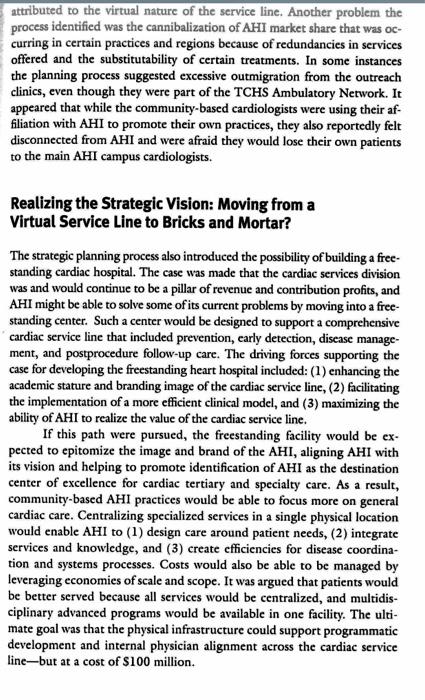
The Case of Amanda Jones wehulance by of the emergency depurtincent +EDy of Fee lise thinenit? time hot wa a mamor of life and dourfi, is was a rack againt time cindinileng and cantias segry and oummurication amoog the ctinkcal leadon wort Liter wiahere brain we lucirt itumage East Bay University Hospital and the American Heart Institute Cardiac Service Line wh dine no hoenc caskis retrokll diniov thit ane furt of I6. Hsi amtula The mission of AHI is to provide world-class, comprehensive cardiac care, to advance cardiac research, and to promote medical education in a fiscally responsible manner. Its vision is to become a premier center of excellence in cardiovascular medicine in the United States. Cardiology and cardiac surgery are to be coordinated in an integrated and seamlesm delivery system. The AHI's goals and guiding principles are - to foster clinical leadership and clinical expertise in high-quality cardiac carc, - to promote a patient-centered care environment and a culture of exectlence, - to develop and implement evidenced-based guidelines that are measurable and outcomes driven, - to provide patients with appropriate education to empower thern and their families to participate in their clinical decision making and self. management, and - to create marketing initiatives that will brand the identity of AHI. AHI Structure AHI is, in practice. a tirtual service linc, requiring ssnerghtic cooperation frum all ICHS candiac services to realiec its mivion and achicte its gouls isec EI. hitvit 111.101, Acrom. AHI the involved carfiac Mrtices indode gencral and intcricntional cardiologs: clectrophysiolugt: the congestive heart failure (CHF) program: cardiac rehabilitation: and cardiac surgery, inctoding carfiac bypus surgen, the minimallv invave vahe urgent program, molvitios surgery, the endoravcular aortic repair eenter. and heart transiant. The mait divioions the consituse the AHIl werike line are canticloge and canfothorade varger:- Theve divivins anc embedded within traditiond deparmontal striturs within the depurtments of medicine ise Evhibit III 11 s and serpery cardiothoracic vergery ane maintained throygh their depurtmunt Howere, AHI under the AHI hirtusl ervice line sricture, deypite the depurtment of onginh "Prrsician Aebulatory Peactices includes oulveach clinica. EXHIBIT III.13 Summary of Statistics (Inctudes East Bay University Hospiral and Truc Cane North Hospital) EXHIBIT III.13 Summary of Statistics (continued) The executive director of AHI, Sandra Getty, BSN, RN, MBA, is respomsible for service line business development and serves as the liaison for cardicnascu. lar programs. She previously worked as the nurw manager in the catheteriza. tion lab with 10. Mount 20 years ago and played a major part in helping the division to become filmless, Since then. Getty has established an clectroplryx. ologv program, including an atrial fibrillation center and a conpective heart failure program. In her current role she is responsible for operational leadership and reriew of compliance activitics, coordination of operations and budget formation for all cost center (cacept for candiothoracic sargery), capital improvements, and expansion planning, including transition details. Getty has alwo been responsible for the acquisition and deiclopment of the community outreach centers throtigh a series of purchakc of group practices; as a resuit. multiple plyasicians are fully emploved to the healtheare sistem. Nom; ste is leading on-boarding cfforts for the new community physician practices. hoping to facilitafe veamless transitions and maintain efficiencics in processes ant care coordination. Cictt has a key respensibility to make sure that all of the proggrams within the eardionascular service line are collctindy marketed under the AHI brand. In addition, all the nume managers and pratice adminiotrator in the cardiothorack intensive care uat ( (IIC L), cardiac intensine carc anit (C(W), and step-down and telemetry units report to her. Recently; she led the implementation of an cloctronic health record system, including computcrized physician order cutry capability for the divi sions of carfiology and carfiothoracic surgery, in foth the ourpatient and inpaticnt settings. She was also responsible for implementing the American College of Cardiology (ACC) National Carduwawcular 1)ata Registry, and the Socicty of Thoracic Surgeons-approxed clectronic datahawes that had becn recommended to track paticnt outcomes. Cictry is very cager to use the new health information toclmwogics (HT) and systems to cnable tracking of paticnt ouscones deroms the AHI service line. By far Gictty's biggest challenge is managing relationships with phycian leadership and AHI faculty: The lack of cocperation among physicians. partially atmibutable to the currenty sirnaal organizational structure for the AHI wrvice line, limits lier cfforts to improne standardization and coondinare sare actos EBCH and the TClfS despite her secess implementing HIT and data rtgistrics. Dr. Cusimano, chicf of cardiothoracic surgery, is considered a national leader in the area of cardiovascular quality improverment. He was recruited rwo years ago from the northeast, in part because of his reputation for quality improvement. Dr. Cusimano has been part of a consortium that includes cardiothoracic surgeons, interventional cardiologists, administrators, perfusionists, anesthesiologists, and operating room and cardiac ICU nurses; this consortium has been actively revicwing the managenent of cardiac discase in the region to identify quality improvement opportunities. For more than 20 years, the consortium has established and maintained registries and collectively developed ways to continuously improve the quality, effectiveness, and costs of care in delivering interventions for patients with cardiac disease. Dr. Cusimano has also played a national role in the Society of Thoracic Surgeons (STS), the national organization for cardiothoracic surgeons; with the STS, he has served as a key member of multiple executive committees. Since coming to EBUH, Dr. Cusimano has tried to establich several multidisciplinary teams and process improvement initiatives. He strongly believes in improving patient outcomnes, not just as a necessary response to increased scrutiny of programs by the state department of health but because it can also address the current AHI problems associated with outmigration of patients and decreases in paticne volume. AHI is proud of its recent statepublished outcomes, including 2 percent mortality in coronary artery bypass graft ( CABG) surgery and a higher than 99.5 percent cath/ PCl survival rate in the catheterization lab. The improvements in CABG surgery, in particular, bave been particularly evident since the arrival of Dr. Cusimano. However, AHI still needs to focus on reducing mortality rates associated with valve strgerics. Despite Dr. Cusimano's national prestige and experience with quality improvement, the current cardiothoracic surgery faculty at EBUH have not embraced the changes he has made. In fact, because all of the other EBUH surgeons were formerly trainees mentored by the current chair of surgery, Dr. Craftman, many are leery of the "new guy." Interestingly, several surgeons had noted that they believed there were already too many cardiac surgeons Cusimano into their group. For the past two years, Dr. Cusimano has attempted to organize the group of cardiac surgeons. He has established multiple teaching and quality forums-including cnhancing the structure, participation, and transparency of the morbidity and mortality conference mectings, and increasing clinic and didactic imolvement with residents and on multidisciplinary rounds. The performance impronement mectings that revicw paticnt complications are now more structured, and processes to address opportunitics for spstematic solutions on the busis of root-cause analises have been dereloped. In general, the tone of care quality review meetings has changed from a focus on faultfinding and berating indiniduak for mistakes to one of sollective effurts to find opportunitics for improsement. Dr. Cusimano has also worked with Dr. Mlount to develop a daily conference session for faculty from cardiology and cardiothoracic sargery during which faculty mect in the catheterization lab to rericw all the operative cases againt recommendations from the ACC:/American Hears Association guidelines prior to performing any surgeries. The objective of this multidisciplinary forum is to cahance the plysicians" ahilities to assess risk and determine appropriate treatments for patients in a collaborative cnvironment. However, many of the cardiothoracic sargcons do not consistently attend the conferences, often sending a resident physician or physician asistant as their representative to present the surgical case under consideration. In the area of HIT-facilitated clinical decision making. Geter and 1.r. Cusimano recently implemented a scrics of imputicat onder sers and chidence based guidelines in the CTICU, step-donn, and telemerry units. As a result of this process, they also decided to incorporate the division's monthly quality indicators into the AHI service line dashbourd (wee Exhibit III. 14). Unfortunately, this lescl of transparency in reporting quality data has not helped improve 13r. Cuvimano's reputation with his colleagoes. De. Cusimano's lack of history with the existing faculty and wxak reiationkipo within EBCH have limited his ability to build volume and a strong neferral bave, thereby minimizing his ovn clinical productivity, As a rosult, the surgeons who operare the most use the newhy avilable patient data to toit their own performance, forther discounting the value of Dr. Cusimano's contributicons to E.LLH. Overall, 19. Cusimano strives to tinite, motivate, and bold exch of the independent cardiac surgcons accotmtable, but be has yet to he succenful in this endeavor. Onc isue he has cncurterd ib that the cmplomment contracts of the surgeous are not uniforth in structure. Dr. Cusimano has proponed to the csecutive administration that each phwician rective a bue silary and then be given an atgementation-ot honm-based on certain metrios isec Evhibit III.151. The measurs would lec reounciled throogh the degurment of tinate on a quartcty bucis. In response to this proposal, the cantiac surgcons recently met prisatcly with the executive administration of EBL'H and the chair of surgery and threatened to lesse the organization. The administration's reaction was to increase the salaries of these surgeons because they were afraid that a large volume of surgical referrals and cases would be diverted to hospital competitors if this group of surgeons left EBUH-but this reaction clearly undermined Dr. Cusimano's individual authority within the group. Morcover, looking ahead, physicians have no direet incentive to align themselves with EBUH's or TCHS's long-term goals, and this does not bode well for future collaboration efforts. EXHIBIT I11.15 Candiac Surgcon Comperiation Model Division of Cardiothoracic Surgery Compensation Model Additional Challenges for the AHI Service Line Dr. Mount and the other members of the cardiac advisory boand recognize that procedures have become less profitable in recent years. Increases in costs combincd with high utilization of costly devices, such as drug-eluting stents and implantable cardioverter defibrillators, have contributed to this problem. Servioe line growth is a perpetual struggle and is influenced by a variety of factors, including shifts in patient volume from inpatient to outpatient treatments; competition across disctiplines, such as cardiology, vascular surgery, and interventional radiology; and the incorporation of novel technologies, such as drug-eluting stents, that led to severe reductions in cardiac surgery volume. In addition, these cost and growth challenges are exacerbated by additional operational and clinical issues. For instance, AHI does not have a single budget because of its design as a virtual service line. Similarly, because of the considerable variability in the particular conditions of each physician's employment contract, expectations and the level of commitment between surgeons and AHI also vary; only some of the cardiac surgeons are fully employed by the bealth system, and many of the contracted surgeons feel lower levels of loyalty to AHI and the health system than AHI would like to have. Finally, as is the case in most healtheare settings, internists and cardiologists follow referral patterns based on their long-lasting relationships; because many of these individuals trained as resident physicians together, they are inclined to refer to the colleagues they know rather than follow AHI criteria for ordering consults or following the on-call schedule. Geographic limitations also pose challenges to the coordination of patients for AHI. Because the building infrastructure was built to accommodate traditional hospital departmental structures, the cardiac surgery practices, CTICU, and operating rooms are contiguous with the department of surgery and division of general surgery. However, these areas are distant (i.c.. floors away) from the cardiology suites that include echocardiography, clectrophysiology, the CCL, and the catheterization labs. Without centralization of services, communication between and among the various entities is complicated; this plysical structure thus reinforces independent silos of activities rather than fostering collaboration throughout AHI. In addition, many of the cardiology group practices are located on different sites around campus. Way-finding for patients is confusing, and the teed to improve coordination of care is further compounded. Despire these challenges, though, the cardiac advisory board believes that a comprehensive and highly specialized heart institute that includes advanced programs will lead to profits down the road. For instance, both Drs. Mount and Cusimano belicve that the division of cardiothoracic surgery needs to develop its minimally invasive vatve surgery program. This need has become especially pressing as the solume of CABG surgerici performed through AHI has plateaued; it appears that many patients are bcing referred by community-based phyicians to the competitor teaching hospital in the city rather than being went to AHI surgeons. In comparisen with the risks aswociated with traditicmal surgery, patients benefit from minimally imsasive value surgery because the breastbone is not split, the rrsk of infection and blecding is lower, hospitil length of stay is shorter. re cinery time in accelerated, and the cosmetic result of the surgery is better, A strong minimally invasive valoe surgery program at AHI would allow AHI to differentiate its product from other hospital competitors that do hot offer this surgteal alternative. Strategic Planning for AHI During the spring of 2010 , the sxecutive adminiktration of TC CS requested that AHI conduct a strategic plan aswesment for 2011-2015. Comsidering the market whare parameters that vere analyzed-incluating population growth, total population si/c, inpaticnt and oatpaticnt market share, phycician stpply and demand. pace mix, and the Ilerfindhal-Hirmchman Ioder ia meastre of markct concentration - capacity for grumth and market prioritization were identificd as primary areas for strategic focus. Additional priotitics include the follising: - Establishing a diveachascd arganization - Creating an outrcach tcam - Buiding progerammatic infrastracture in the congestise heart failure and chectophysiolosy departments - Fepanding the AHI outrcach clinis nemuork - Expanding the candiac rehab program - Heceloping parmerships with targeted local and regional communiry cardiodogy practices - Increasing Truc Care Ambulatory Network refcrtals to AHI phrsiciams - Establishing a onc-stop communisations othice - L'sing paticat hacigators and antrcach cororfinators to serse as the comsectors between AHII plasicians, rstorting community- hased plysicians, and paticats Results of the stratcegie plannine prosess aloo highlighted the toranding problem of the AHI and noted that mach of the problem soukd te attributed to the virtual nature of the service line. Another problem the process identified was the cannibalization of AHI market share that was occurring in certain practices and regions becauke of redundancies in services offered and the substitutability of certain treatmens. In some instances the planning process suggested excessive outmigration from the outreach clinics, even though they were part of the TCHS Ambulatory Network. It appeared that while the community-based cardiologists were using their affiliation with AHI to promote their own practices, they also reportedly felt disconnected from AHI and were afraid they would lose their own patients to the main AHI campus cardiologists. Realizing the Strategic Vision: Moving from a Virtual Service Line to Bricks and Mortar? The strategic planning proces also introduced the ponsiblity of builifing a frecstanding cardiac hospital. The case was made that the cardiac services division was and would continue to be a pillar of revenue and contribution profits, and AHI might be able to solve some of its current problems by mowing into a freestanding center. Such a center would be designed to support a comprehensive candiac service line that induded prevention, eanly detection, disease management, and postprocedure follow-up care. The driving forces supporting the case for developing the freestanding heart hospital indluded: (1) enhancing the academic stature and branding image of the cardiac service line, (2) facilituting the implementation of a more efficient clinical model, and (3) maximizing the ability of AHI to realize the value of the cartiinc scrvice line. If this path were pursued, the freestanding facility would be ex. pected to epitomize the image and brand of the AHI, aligning AHI with its vision and belping to promote identification of AHI as the destination center of excellence for cardiac tertiary and specialry care. As a resultr, community-based AHI practices would be able to focus more on general cardiac care. Centralizing specialized services in a single physical location would enable AHt to (1) design care around patient needs, (2) integrate services and knowedge, and (3) create efficiencies for disease coordination and systems processes. Costs would also be able to be managed by leveraging economies of scale and scope. It was argued that patients would be better served because all services would be eentralized, and multidis: ciplinary advanced programs would be avallable in one facility. The ultimate goal was that the physical infrastructure could support programmatic development and internal physician alignment acrost the cardiac service line-but at a cost of $100 million. Conclusion At present, AHI leadership must sort out the service line situation and the alternatives ahead. Fortunatcly the clear consensus is that patients like Amanda Jones cannot suffer from poor sertice or poor care quality because of issues related to problems with misaligned incentives, poor collaboration, or inadequate coordination. 1.cadership realizes that it must continue to proride both clinical and nonclinical staff with the resources and cducation tools ther need to be able to provide the best care possible. Yet introducing some of these resources and tools has proved ditficult in many circumstances. Neither the employecs nor the staff should get caught up in the challenges affecting the service line, but even under the most optimistic of circumstances, a new build. ing for the AHI would not be arailable until 2015. Case Questions 1. What problems and issues result from the way AHI is currently organized: 2. How are design issues esacerbated by power contlicts between and among physicians 3. What are the issues that a new building for AHI mighe be able to solee: What issues might still plaguc AHI: 4. What would you recommend that AHll leaderhip do now? Who would you inole in making decisions about the future for AHI? Case H The American Heart Institute Sofia V. Agoritsas and Ann Scheck McAlearney The Case of Amanda Jones Presenting with chest pain, 60-year-old Amanda Jones was rushed from the ambulance bay of the emergency department (ED) of Fast Bay University Hospital (EBUH) to the catheterization lab. The American Heart Institute (AHI) lab team determined that Jones was experiencing an ST-scgment eleration myocardial infarction (STEMI), the deadliest type of heart attack. As a result, within 30 minutes of her arrival, Jones reecived a percutaneous coronary intervention (PCI), but the occluded artery could not be opened. The cardiac catheterization lab team accelerated the protocols to fasttrack Jones for emergency cardiac bypass surgery with the cardiac surgeon on call. I.uckily; Joseph Cusimano, MD, the chief of cardiac surgery, was available, and Jones was taken into the operating room (OR) within one hour. As time lost was a matter of life and death, it was a race against time. Collaboration among the interdisciplinary teams of the divisions of cardiology and cardiac surgery and communication among the clinical leaders throughout the AHI were critical to Jones's survival. Fortunately for Jones, her cardiac cmergency had a happy ending. She recovered and was released a week later without brain or heart damage. What Jones didn't know, though, was that AHI was more of a virtual institute than an actual place. Although she had been seen and treated at FBUH, the collaboration and communication that occurred crossed departments, divisions, and organizational berundaries. And unfortunatcly. AHI's executive director Sandra Cictty was not convinced that this structure alwals prowided paticnts and their familics with the best care and service quality they expected and deserved. East Bay University Hospital and the American Heart Institute Cardiac Service Line FBUH, a 700-bed teaching hospital, is one of two tertiary care facilities within True Care Health System (TCHSI. FBUH is the flaghhip hospital for adult acute care in the health system. The other acute care hespital, True Care North, was only recently acquired by TCHS and is 20 miles away from the other four main facilities. The Children's Hospital, a psycthiatric hospital, and a cancer hospital constitute the remaining three hospitals of ICHS. AHI is the cardiac service line that spans TCHS. AHI is vicwed as a leading provider and pieneer in cardiac care in the region. It is led be Dr. Barry A. Mount, an interientional cardiologist. AHI proxides adult cardiac care throughout the state and includes a staff of 50 full-time emplowed cardiologists and cight cardiac surgecons, five of whom primarily work out of EBUH isee Fxhibits 111.8 and 1II.9). The AHI service line also includes six close-to-home cartiac outreach clinics that are part of ICHS's ambulatory carc network: this network spans the suburbs around the five-hospital health system. AHI has been listed nationally by lcading organizations such as Healthgrades as a top-ranking cardiac program in the L'nited Stares, but it has not yet been ranked as a top program in L.S. Nenrs o Ilirid Report. The mission of AHI is to provide world-class, comprehensive cardiac care, to advance cardiac research, and to promote medical education in a fiscally responsible manner. Its vision is to become a premier center of excellence in cardiovascular medicine in the United States. Cardiology and cardiac surgery are to be coordinated in an integrated and seamless delivery system. The AHI's goals and guiding principles are - to foster clinical leadership and clinical expertise in high-quality cardiac care, - to promote a patient-centered care environment and a culture of excellence, - to develop and implement evidenced-based guidelines that are measurable and outcomes driven, - to provide patients with appropriate education to empower them and their families to participate in their clinical decision making and selfmanagement, and - to create marketing initiatives that will brand the identity of AHI. AHI is, in practice, a virtual service line, requiring synergistic cooperation from all TCHS cardiac services to realize its mission and achieve its goals isee Fxhibit III.101. Across. AHI the involved cardiac services include general and interventional cardiology: electrophrisiology; the congestive heart failure (C:HF) program; cardiac rehabilitation; and cardiac surgery; including cardiac bepass surgery, the minimally invasive valse surgery program. robotics surgery, the endowaetular aortic repair center, and heart transplant. The main divisions that constitute the AHI service line are cardiology and cardiothoracic surgery. These disisioms are embedded within traditional departmental structures within the department of medicine (see Exhibit III.11, and surgery Fee Exhibit III,121. As a result, budectary control of the divisions of cardiology and cardiththoracic surgery are maintained through their depurtments. Howewer. AHI srvice line prolit and less statements and summary of statistics reports isee Exhilvit III.13) are revicued monthly by an . AHI cardiac athisery boand. Furthermore, marketing activitics incorporate advertiving for cardiology and cardiothoracic surgery under the AHI virtual service line structure, despite the depurtment of origin. "Physiclan Ambulatery Practices includes outreach clinics. XHIBIT III.13 Summary of Statistics (Includes East Bay University Hospital and Truc Care North Hospital) EXHIBIT III.13 Summary of Statistics (continued) Leadership Challenges for the AHI Service Line The executive director of AHI, Sandra Getty, BSN, RN, MIBA, is responsible for service line business development and serves as the liaison for cardionascular programs. She previously worked as the nurse manager in the catheterization lab with Dr. Mount 20 years ago and played a major part in helping the division to become filmless. Since then, Getty has established an electrophysiology program, including an atrial fibrillation center and a congestive heart failure program. In her current role she is responsible for operational leadership and review of compliance activities, coordination of operations and budget formation for all cost centers (except for cardiothoracic surgery), capital improvements, and expansion planning, including transition details. Getty has also been responsible for the acquisition and derelopment of the community outreach centers through a serics of purchases of group practices; as a result, multiple physicians are fully employed by the healtheare system. Now, she is leading on-boarding efforts for the new community physician practices, hoping to facilitate seamless transitions and maintain efficiencies in processes and care coordination. Cictty has a key responsibility to make sure that all of the programs within the cardiovascular service line are collectively marketed under the AHI brand. In addition, all the nurse managers and practice administrators in the cardiothoracic intensive care unit (CTICL?), cardiac intensive care unit (C.CU), and step-down and telemetry units report to her. Recently, she led the implementation of an electronic health record system, including computerized physician order entry capability for the divisions of cardiology and cardiothoracic surgery, in both the outpatient and inpatient settings. She was also responsible for implementing the American College of (ardiology (ACC) National Cardiosascular Data Registry, and the Society of Thoracic Surgeons-approxed electronic databases that had been recommended to track patient outcomes. Gietty is very eager to use the new health information techologics ( HIT) and systems to cnable tracking of patient outcomes across the AHI service line. By far Cietty's biggest challenge is managing relationships with phsician leadership and AHI faculty: The lack of cooperation among physicians. partially attributable to the currently virtual organizational structure for the AHI scrvice line, limits her cfforts to improve standardization and coordinate care across FBLH and the TCHS-despite her success implementing HIT and data registrics. Quality Improvement Challenges for the AHI Service Line Dr. Cusimano, chief of cardiothoracic surgery, is considered a national leader in the area of cardiovascular quality improvement. He was recruited two years ago from the northeast, in part because of his reputation for quality improvement. Dr. Cusimano has been part of a consortium that includes cardiothoracic surgeons, interventional cardiologists, administrators, perfusionists, anesthesiologists, and operating room and cardiac ICU nurses; this consortium has been actively reviewing the management of cardiac disease in the region to identify quality improvement opportunities. For more than 20 years, the consortium has established and maintained registries and collectively developed ways to continuously improve the quality, effectiveness, and costs of care in delivering interventions for patients with cardiac disease. Dr. Cusimano has also played a national role in the Society of Thoracic Surgeons (STS), the national organization for cardiothoracic surgeons; with the STS, he has served as a key member of multiple executive committees. Since coming to EBUH, Dr. Cusimano has tried to establish several multidisciplinary teams and process improvement initiatives. He strongly believes in improving patient outcomes, not just as a necessary response to increased scrutiny of programs by the state department of health but because it can also address the current AHI problems associated with outmigration of patients and decreases in patient volume. AHI is proud of its recent statepublished outcomes, including 2 percent mortality in coronary artery bypass graft (CABG) surgery and a higher than 99.5 percent cath/PCI survival rate in the catheterization lab. The improvements in CABG surgery, in particular, have been particularly evident since the arrival of Dr. Cusimano. However, AHI still needs to focus on reducing mortality rates associated with valve surgeries. Despite Dr. Cusimano's national prestige and experience with quality improvement, the current cardiothoracic surgery faculty at EBUH have not embraced the changes he has made. In fact, because all of the other EBUH surgeons were formerly trainees mentored by the current chair of surgery, Dr. Craftman, many are leery of the "new guy." Interestingly, several surgeons had noted that they believed there were already too many cardiae surgeons on staff at EBUH, so they were predictably unenthusiastic about bringing Dr. Cusimano into their group. For the past two years, Dr. Cusimano has attempted to organize the group of cardiac surgeons. He has established multiple teaching and quality forums-including enhancing the structure, participation, and transparency of the morbidity and mortality conference meetings, and increasing clinic and didactic involvement with residents and on multidisciplinary rounds. The performance improvement meetings that review patient complications are now more structured, and processes to address opportunities for systematic solutions on the basis of root-cause analyses have been developed. In general, the tone of care quality review meetings has changed from a focus on faultfinding and berating individuals for mistakes to one of collective efforts to find opportunities for improvement. Dr. Cusimano has also worked with Dr. Mount to develop a daily conference session for faculty from cardiology and cardiothoracic surgery during which faculty meet in the catheterization lab to review all the operative cases against recommendations from the ACC/American Heart Association guidelines prior to performing any surgeries. The objective of this multidisciplinary forum is to enhance the physicians' abilities to assess risk and determine appropriate treatments for patients in a collaborative environment. However, many of the cardiothoracic surgeons do not consistently attend the conferences, often sending a resident physician or phyysician assistant as their representative to present the surgical case under consideration. In the area of HIT-facilitated clinical decision making, Getty and Dr. Cusimano recently implemented a serics of inpatient order sets and evidence-based guidelines in the CTICU, step-down, and telemetry units. As a result of this process, they also decided to incorporate the division's monthly quality indicators into the AHI service line dashboand (see Exhibit III.14). Unfortunately, this level of transparency in reporting quality data has not helped improve Dr. Cusimano's reputation with his colleagues. Dr. Cusimano's lack of history with the existing faculty and weak relationships within EBUH have limited his ability to build rolume and a strong referral base, thereby minimizing his own clinical productivit. As a result, the surgeons who operate the most use the newly arailable patient data to tout their own performance, further discounting the value of Dr. Cusimano's contributions to EBUH. Overall, Dr. (isimano strives to unite, motivate, and hold each of the independent cardiac surgeons accountable, but he has yet to be successful in this endeavor. One issuc he has encountered is that the employment contracts of the surgeons are not uniform in structure. Dr. Cusimano has proposed to the executive administration that each physician receive a base salary and then be given an augmentation-or bonus-hased on certain metrics (see Exhibit III.151. The measures would he reconciled through the department of finance on a quarterly basis. In response to this proposal, the candiac surgeons recently met privately with the executive administration of EBUH and the chair of surgery and threatened to leave the organization. The administration's Performance Metrics Dashboard reaction was to increase the salaries of these surgeons because they were afraid that a large volume of surgical referrals and cases would be diverted to hospital competitors if this group of surgeons left EBUH-but this reaction clearly undermined Dr. Cusimano's individual authority within the group. Moreover, looking ahead, physicians have no direct incentive to align themselves with EBUH's or TCHS's long-term goals, and this does not bode well for future collaboration efforts. EXHIBIT III.15 Cardiac Surgeon Compensation Model Division of Cardiothoracic Surgery Compensation Model Surgeon: Augmentation Schedule Above Base Salary: Additional Challenges for the AHI Service Line Dr. Mount and the other members of the cardiac advisory board recognize that procedures have become less profitable in recent years. Increases in costs combined with high utilization of costly devices, such as drug-eluting stents and implantable cardioverter defibrillators, have contributed to this problem. Service line growth is a perpetual struggle and is influenced by a variety of factors, including shifts in patient volume from inpatient to outpatient treatments; competition across disciplines, such as cardiology, vascular surgery, and interventional radiology; and the incorporation of novel technologies, such as drug-eluting stents, that led to severe reductions in cardiac surgery volume. In addition, these cost and growth challenges are exacerbated by additional operational and clinical issues. For instance, AHI does not have a single budget because of its design as a virtual service line. Similarly, because of the considerable variability in the particular conditions of each physician's employment contract, expectations and the level of commitment between surgeons and AHI also vary; only some of the cardiac surgeons are fully employed by the health system, and many of the contracted surgeons feel lower levels of loyalty to AHI and the health system than AHI would like to have. Finally, as is the case in most healthcare settings, internists and cardiologists follow referral patterns based on their long-lasting relationships; because many of these individuals trained as resident physicians together, they are inclined to refer to the colleagues they know rather than follow AHI criteria for ordering consults or following the on-call schedule. Geographic limitations also pose challenges to the coordination of patients for AHI. Because the building infrastructure was built to accommodate traditional hospital departmental structures, the cardiac surgery practices, CTICU, and operating rooms are contiguous with the department of surgery and division of general surgery. However, these areas are distant (i.e., floors away) from the cardiology suites that include echocardiography, electrophysiology, the CCU, and the catheterization labs. Without centralization of services, communication between and among the various entities is complicated; this physical structure thus reinforces independent silos of activities rather than fostering collaboration throughout AHI. In addition, many of the cardiology group practices are located on different sites around campus. Way-finding for patients is confusing, and the need to improve coordination of care is further compounded. Despite these challenges, though, the cardiac advisory board believes that a comprehensive and highly specialized heart institute that includes advanced programs will lead to profits down the road. For instance, both Drs. Mount and Cusimano believe that the division of cardiothoracic surgery needs to develop its minimally invasive valve surgery program. This need has become especially pressing as the volume of CABG surgeries performed through AHI has plateaued; it appears that many patients are being referred by community-based physicians to the comperitor teaching hospital in the city rather than being sent to AHI surgeons. In comparison with the risks associated with traditional surgery; patients benefit from minimally invasive valve surgery because the breastbone is not split, the risk of infection and bleeding is lower, hospital length of stay is shorter, recovery time is accelerated, and the cosmetic result of the surgery is better. A strong minimally invasive valse surgery program at AHI would allow AHI to differentiate its product from other hospital competitors that do not offer this surgical alternative. Strategic Planning for AHI D)uring the spring of 2010, the executive administration of TCHS requested that AHI conduct a strategic plan assessment for 2011-2015. Considering the market share parameters that were analyzed-including population growth, total population size, inpatient and outpaticnt market share, phsician supply and demand. parer mix, and the Ilerfindhal-Hirschman Index (a measure of market concentration-capacity for growth and market prioritization were identificd as primary arcas for strategic focus. Additional prioritics include the following: - Establishing a discasc-bascd organization - Creating an outreach team - Building programmatic infrastructure in the congestive heart failure and clectrophyisiology departments - Fxpanding the AHI outreach clinic nctwork - Fxpanding the cardiac rehab program - 1Developing partnerships with targeted local and regional community cardiology practices - Increasing Truc Care Ambulatory Network referrals to AHI phyisicians - Establishing a one-stop communications office - L'sing paticnt naxigators and outreach coordinaton to serie as the connectors between AHII physicians, referring community-hased physicians, and paticnts Results of the strategic planning process also highlighted the branding problem of the AHI and noted that much of the problem could be attributed to the virtual nature of the service line. Another problem the process identified was the cannibalization of AHI market share that was occurring in certain practices and regions because of redundancies in services offered and the substitutability of certain treatments. In some instances the planning process suggested excessive outmigration from the outreach clinics, even though they were part of the TCHS Ambulatory Network. It appeared that while the community-based cardiologists were using their affiliation with AHI to promote their own practices, they also reportedly felt disconnected from AHI and were afraid they would lose their own patients to the main AHI campus cardiologists. Realizing the Strategic Vision: Moving from a Virtual Service Line to Bricks and Mortar? The strategic planning process also introduced the possibility of building a freestanding cardiac hospital. The case was made that the cardiac services division was and would continue to be a pillar of revenue and contribution profits, and AHI might be able to solve some of its current problems by moving into a freestanding center. Such a center would be designed to support a comprehensive cardiac service line that included prevention, early detection, disease management, and postprocedure follow-up care. The driving forces supporting the case for developing the freestanding heart hospital included: (1) enhancing the academic stature and branding image of the cardiac service line, (2) facilitating the implementation of a more efficient clinical model, and (3) maximizing the ability of AHI to realize the value of the cardiac service line. If this path were pursued, the freestanding facility would be expected to epitomize the image and brand of the AHI, aligning AHI with its vision and helping to promote identification of AHI as the destination center of excellence for cardiac tertiary and specialty care. As a result, community-based AHI practices would be able to focus more on general cardiac care. Centralizing specialized services in a single physical location would enable AHI to (1) design care around patient needs, (2) integrate services and knowledge, and (3) create efficiencies for disease coordination and systems processes. Costs would also be able to be managed by leveraging economies of scale and scope. It was argued that patients would be better served because all services would be centralized, and multidisciplinary advanced programs would be available in one facility. The ultimate goal was that the physical infrastructure could support programmatic development and internal physician alignment across the cardiac service line-but at a cost of $100 million. At present, AHI leadership must sort out the service line situation and the alternatives ahead. Fortunately the clear consensus is that patients like Amanda Jones cannot sufter from poor service or poor care quality because of issues related to problems with misaligned incentives, poor collaboration, or inadequate coordination. 1.eadership realizes that it must continue to provide both clinical and nonclinical staff with the resources and education tools ther need to be able to provide the hest care possible. let introducing some of these resources and tools has proved difficult in many circumstances. Neither the employees nor the staff should get caught up in the challenges affecting the service line, but even under the most optimistic of circumstances, a new building for the AHI would not be wailable until 2015. Case Questions 1. What problems and issues result from the way AIH is currently organized: 2. How are design issues exacerbated by power conflicts between and among physicians? 3. What are the issues that a new building for AHI might be able to solve: What isstes might still plague AIII? 4. What would you recommend that AHI lcadership do now? Who would you inole in making decisions about the future for AHI? Case H The American Heart Institute Sofia V. Agoritsas and Ann Scheck McAlearney The Case of Amanda Jones Presenting with chest pain, 60-year-old Amanda Jones was rushed from the ambulance bay of the emergency department (ED) of Fast Bay University Hospital (EBUH) to the catheterization lab. The American Heart Institute The mission of AHI is to provide world-class, comprehensive eardiac care, to advance cardiac research, and to promote medical education in a fiscally responsible manner. Its vision is to become a premier center of excellence in cardiovascular medicine in the United States. Cardiology and cardiac surgery are to be coordinated in an integrated and seamless delivery system. The AHI's goals and guiding principles are - to foster clinical leadership and clinical expertise in high-quality cardiac care, - to promote a patient-centered care environment and a culture of excellence, - to develop and implement evidenced-based guidelines that are measurable and outcomes driven, - to provide patients with appropriate education to empower them and their families to participate in their clinical decision making and selfmanagement, and - to create marketing initiatives that will brand the identity of AHI. AHI Structure AHI is, in practice, a virtual service line, requiring synergistic cooperation from all TCHS cardiac services to realize its mission and achieve its goals (sec Fxhibit III.101. Across. AHI the involved cardiac services include general and interventional cardiology: clectrophyiology: the congestive heart failure (C.HF, program; cardiac rehabilitation; and cardiac surgery; including cardiac bypass surgery, the minimally invasive valve surgery program. robotics surgery, the endowasular aortic repair center, and heart transplant. The muin divisions that constitute the AHI service line are cardiology and cardiothoracic surger:. These divisions are embedded within traditional departmental structures within the depurtments of medicine (se Evhibit III.11) and surgery F tee Exhibit 111.12 . As a result, budectary control of the dinisions of cardiology and cardiothoracic surgery are maintained through their department. Howeerr, AHI wervice line profit and loss statements and summary of statistics neports isee Fixhilht III.13) are reviewed monthly by an . Al cardiac axtisory boand. Furthermore, marketing activitics incomporate advertiving for cardiology and cardiothoracic surgery under the AHI virtual service line structure, despite the department of onigin. "Physician Ambulatory Practices includes celtreach clinics. XHIBIT III.13 Summary of Statistics (Includes East Bay University Hospital and True Care North Hospital) EXHIBIT III.13 Summary of Statistics (continued) Leadership Challenges for the AHI Service Line The executive director of AHI, Sandra Getty, BSN, RN, MIBA, is responsible for service line business development and serves as the liaison for cardionascular programs. She previously worked as the nurse manager in the catheterization lab with Dr. Mount 20 years ago and played a major part in helping the division to become filmless. Since then, Getty has established an electrophysiology program, including an atrial fibrillation center and a congestive heart failure program. In her current role she is responsible for operational leadership and review of compliance activities, coordination of operations and budget formation for all cost centers (except for cardiothoracic surgery), capital improvements, and expansion planning, including transition details. Getty has also been responsible for the acquisition and derelopment of the community outreach centers through a serics of purchases of group practices; as a result, multiple physicians are fully employed by the healtheare system. Now, she is leading on-boarding efforts for the new community physician practices, hoping to facilitate seamless transitions and maintain efficiencies in processes and care coordination. Cictty has a key responsibility to make sure that all of the programs within the cardiovascular service line are collectively marketed under the AHI brand. In addition, all the nurse managers and practice administrators in the cardiothoracic intensive care unit (CTICL?), cardiac intensive care unit (C.CU), and step-down and telemetry units report to her. Recently, she led the implementation of an electronic health record system, including computerized physician order entry capability for the divisions of cardiology and cardiothoracic surgery, in both the outpatient and inpatient settings. She was also responsible for implementing the American College of (ardiology (ACC) National Cardiosascular Data Registry, and the Society of Thoracic Surgeons-approxed electronic databases that had been recommended to track patient outcomes. Gietty is very eager to use the new health information techologics ( HIT) and systems to cnable tracking of patient outcomes across the AHI service line. By far Cietty's biggest challenge is managing relationships with phsician leadership and AHI faculty: The lack of cooperation among physicians. partially attributable to the currently virtual organizational structure for the AHI scrvice line, limits her cfforts to improve standardization and coordinate care across FBLH and the TCHS-despite her success implementing HIT and data registrics. Quality Improvement Challenges for the AHI Service Line Dr. Cusimano, chief of cardiothoracic surgery, is considered a national leader in the area of cardiovascular quality improvement. He was recruited two years ago from the northeast, in part because of his reputation for quality improvement. Dr. Cusimano has been part of a consortium that includes cardiothoracic surgeons, interventional cardiologists, administrators, perfusionists, anesthesiologists, and operating room and cardiac ICU nurses; this consortium has been actively reviewing the management of cardiac disease in the region to identify quality improvement opportunities. For more than 20 years, the consortium has established and maintained registries and collectively developed ways to continuously improve the quality, effectiveness, and costs of care in delivering interventions for patients with cardiac disease. Dr. Cusimano has also played a national role in the Society of Thoracic Surgeons (STS), the national organization for cardiothoracic surgeons; with the STS, he has served as a key member of multiple executive committees. Since coming to EBUH, Dr. Cusimano has tried to establish several multidisciplinary teams and process improvement initiatives. He strongly believes in improving patient outcomes, not just as a necessary response to increased scrutiny of programs by the state department of health but because it can also address the current AHI problems associated with outmigration of patients and decreases in patient volume. AHI is proud of its recent statepublished outcomes, including 2 percent mortality in coronary artery bypass graft (CABG) surgery and a higher than 99.5 percent cath/PCI survival rate in the catheterization lab. The improvements in CABG surgery, in particular, have been particularly evident since the arrival of Dr. Cusimano. However, AHI still needs to focus on reducing mortality rates associated with valve surgeries. Despite Dr. Cusimano's national prestige and experience with quality improvement, the current cardiothoracic surgery faculty at EBUH have not embraced the changes he has made. In fact, because all of the other EBUH surgeons were formerly trainees mentored by the current chair of surgery, Dr. Craftman, many are leery of the "new guy." Interestingly, several surgeons had noted that they believed there were already too many cardiae surgeons on staff at EBUH, so they were predictably unenthusiastic about bringing Dr. Cusimano into their group. For the past two years, Dr. Cusimano has attempted to organize the group of cardiac surgeons. He has established multiple teaching and quality forums-including enhancing the structure, participation, and transparency of the morbidity and mortality conference meetings, and increasing clinic and didactic involvement with residents and on multidisciplinary rounds. The performance improvement meetings that review patient complications are now more structured, and processes to address opportunities for systematic solutions on the basis of root-cause analyses have been developed. In general, the tone of care quality review meetings has changed from a focus on faultfinding and berating individuals for mistakes to one of collective efforts to find opportunities for improvement. Dr. Cusimano has also worked with Dr. Mount to develop a daily conference session for faculty from cardiology and cardiothoracic surgery during which faculty meet in the catheterization lab to review all the operative cases against recommendations from the ACC/American Heart Association guidelines prior to performing any surgeries. The objective of this multidisciplinary forum is to enhance the physicians' abilities to assess risk and determine appropriate treatments for patients in a collaborative environment. However, many of the cardiothoracic surgeons do not consistently attend the conferences, often sending a resident physician or phyysician assistant as their representative to present the surgical case under consideration. In the area of HIT-facilitated clinical decision making, Getty and Dr. Cusimano recently implemented a serics of inpatient order sets and evidence-based guidelines in the CTICU, step-down, and telemetry units. As a result of this process, they also decided to incorporate the division's monthly quality indicators into the AHI service line dashboand (see Exhibit III.14). Unfortunately, this level of transparency in reporting quality data has not helped improve Dr. Cusimano's reputation with his colleagues. Dr. Cusimano's lack of history with the existing faculty and weak relationships within EBUH have limited his ability to build rolume and a strong referral base, thereby minimizing his own clinical productivit. As a result, the surgeons who operate the most use the newly arailable patient data to tout their own performance, further discounting the value of Dr. Cusimano's contributions to EBUH. Overall, Dr. (isimano strives to unite, motivate, and hold each of the independent cardiac surgeons accountable, but he has yet to be successful in this endeavor. One issuc he has encountered is that the employment contracts of the surgeons are not uniform in structure. Dr. Cusimano has proposed to the executive administration that each physician receive a base salary and then be given an augmentation-or bonus-hased on certain metrics (see Exhibit III.151. The measures would he reconciled through the department of finance on a quarterly basis. In response to this proposal, the candiac surgeons recently met privately with the executive administration of EBUH and the chair of surgery and threatened to leave the organization. The administration's reaction was to increase the salaries of these surgeons because they were afraid that a large volume of surgical referrals and cases would be diverted to hospital competitors if this group of surgeons left EBUH - but this reaction clearly undermined Dr. Cusimano's individual authority within the group. Moreover, looking ahead, physicians have no direct incentive to align themselves with EBUH's or TCHS's long-term goals, and this does not bode well for future collaboration efforts. EXHIBIT III.15 Cardiac Surgeon Compensation Model Division of Cardiothoracic Surgery Compensation Model Surgeon: Augmentation Schedule Above Base Salary: Additional Challenges for the AHI Service Line Dr. Mount and the other members of the cardiac advisory board recognize that procedures have become less profitable in recent years. Increases in costs combined with high utilization of costly devices, such as drug-eluting stents and implantable cardioverter defibrillators, have contributed to this problem. Service line growth is a perpetual struggle and is influenced by a variety of factors, including shifts in patient volume from inpatient to outpatient treatments; competition across disciplines, such as cardiology, vascular surgery, and interventional radiology; and the incorporation of novel technologies, such as drug-eluting stents, that led to severe reductions in cardiac surgery volume. In addition, these cost and growth challenges are exacerbated by additional operational and clinical issues. For instance, AHI does not have a single budget because of its design as a virtual service line. Similarly, because of the considerable variability in the particular conditions of each physician's employment contract, expectations and the level of commitment between surgeons and AHI also vary; only some of the cardiac surgeons are fully employed by the health system, and many of the contracted surgeons feel lower levels of loyalty to AHI and the health system than AHI would like to have. Finally, as is the case in most healthcare settings, internists and cardiologists follow referral patterns based on their long-lasting relationships; because many of these individuals trained as resident physicians together, they are inclined to refer to the colleagues they know rather than follow AHI criteria for ordering consults or following the on-call schedule. Geographic limitations also pose challenges to the coordination of patients for AHI. Because the building infrastructure was built to accommodate traditional hospital departmental structures, the cardiac surgery practices, CTICU, and operating rooms are contiguous with the department of surgery and division of general surgery. However, these areas are distant (i.e., floors away) from the cardiology suites