Hospitals across the country have seen an increase in Methicillin-resistant Staphylococcus Aureus (MRSA), a bacterial infection that
Question:
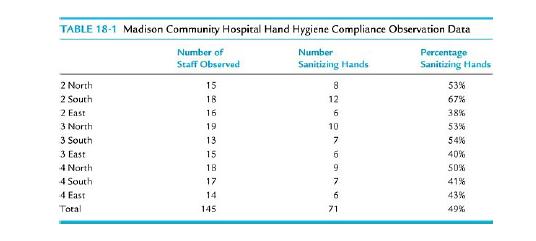
Hospitals across the country have seen an increase in Methicillin-resistant Staphylococcus Aureus (MRSA), a bacterial infection that is highly resistant to some antibiotics. Patients who contract this infection can develop serious complications, sometimes leading to death. Area hospitals with MRSA outbreaks have been featured in recent media programs, resulting in a loss of public confidence and declining admissions. As the director of an inpatient unit at Madison Community Hospital (MCH), you understand the potential for an increase of MRSA at your hospital. Your infectious disease physicians are concerned about the potential for an outbreak at your hospital. Infection prevention studies have reported that only 40% of health care workers sanitize their hands before treating patients. Hand washing and other handsanitizing methods have been proven to reduce the transmission of dangerous infections from one patient to another. The MCH products committee has evaluated several hand-sanitizing products and selected an alcohol-based product that effectively eliminates the majority of bacterial microorganisms that can be transmitted by contact. The hand hygiene policy at MCH requires staff members, physicians, and volunteers to apply the hand sanitizer before entering and after leaving a patient’s room. The Infection Prevention staff estimates an average of 15–20 individuals enter a patient’s room each day. You have been appointed to serve on a task force charged with improving hand hygiene compliance. The Infection Prevention personnel have gathered preliminary data from various inpatient nursing units (see Table 18-1). Staff on these units were observed in order to assess whether they sanitized their hands prior to entering and upon leaving a patient’s room. The Infection Prevention staff observing the inpatient unit personnel are routinely seen on these units as part of their surveillance activities. Staff members were not aware their hand hygiene practices were being observed. At first glance, the data indicates hand hygiene is not practiced, as required by the policy, in more than half the observations.
MCH has adopted the FOCUS-PDCA improvement model and utilizes various tools for collecting data and analyzing processes. The hand hygiene task force will be applying these methods to address the hand hygiene concern.
DISCUSSION QUESTIONS
1. How would your task force use the FOCUS model and the data collection, process mapping, and process analysis tools to plan for a process change?
2. What are some of the issues associated with caregivers sanitizing their hands? Why do you suppose only 40% of caregivers sanitize their hands? What other department personnel, besides nursing, may need to enter a patient’s room during their stay?
3. Who should be on this task force to represent which hospital functions and why? To whom should the task force report their results and why?
4. What are the possible causes for noncompliance? Are there other factors contributing to the issue?
5. What data are needed to determine the factors involved in the noncompliance?
6. How would the problem look different if it turned out only a handful of personnel were noncompliant? How would this affect the improvement process?
7. Do you have enough data to complete the analysis? What data are needed to determine the factors involved in the noncompliance?
8. What process should be selected for improvement?
9. What aspects of the FOCUS model would be most useful to target the improvement efforts?
10. How can MCH motivate its staff to be more compliant? Do you think posters and recognition awards for units with the best results would help move the numbers in the right direction? Why or why not?
11. What do you think about the idea of installing a poka-yoke, that is, an engineering approach to prevent an error before it occurs?
Step by Step Answer:

Introduction To Health Care Management
ISBN: 9781284081015
3rd Edition
Authors: Sharon B. Buchbinder, Nancy H. Shanks